Proteins serve as the building blocks of life and perform tasks essential to maintaining a cell. To perform these tasks, they must fold into specific conformations. However, proteins can also misfold and become infectious. These types of proteins are called prions, and they can cause other proteins to also misfold, a method of self-replication that resembles that of viruses. Prions are especially spine chilling because they are resistant to heat, chemicals, and even radiation. In fact, a recent study showed that the prion involved in multiple system atrophy (MSA) might be transmissible on surgical tools. Immediately, this incited questions about whether standard hospital disinfecting techniques are sufficient.
Prions were first discovered in the 1980s. Stanley Prusiner coined the term after showing that misfolded proteins were functioning as infectious agents and causing Creutzfeldt-Jakob Disease (CJD). CJD is a slow, progressive neurodegenerative disease transmitted to humans following their consumption of beef from cattle with the infamous mad cow disease. Skeptics of prions tried to prove Prusiner wrong, unable to fathom how a protein could replicate without following the central dogma of biology. Even the simplest viruses contain the genetic material needed to reproduce.
But further evidence since this discovery has supported the idea that a protein alone can transmit disease. In a recent study led by Kurt Giles, associate professor of neurology at the University of California, San Francisco, a newly discovered prion called alpha-synuclein was shown to cause MSA.
MSA is characterized by the progressive loss of function and death of nerves in the central nervous system. To test if MSA could be transmitted by prions, Giles exposed a group of mice to the brain tissue of human MSA patients. These mice displayed neurodegeneration, leading the scientists to conclude that MSA was being transmitted from human tissue to mice.
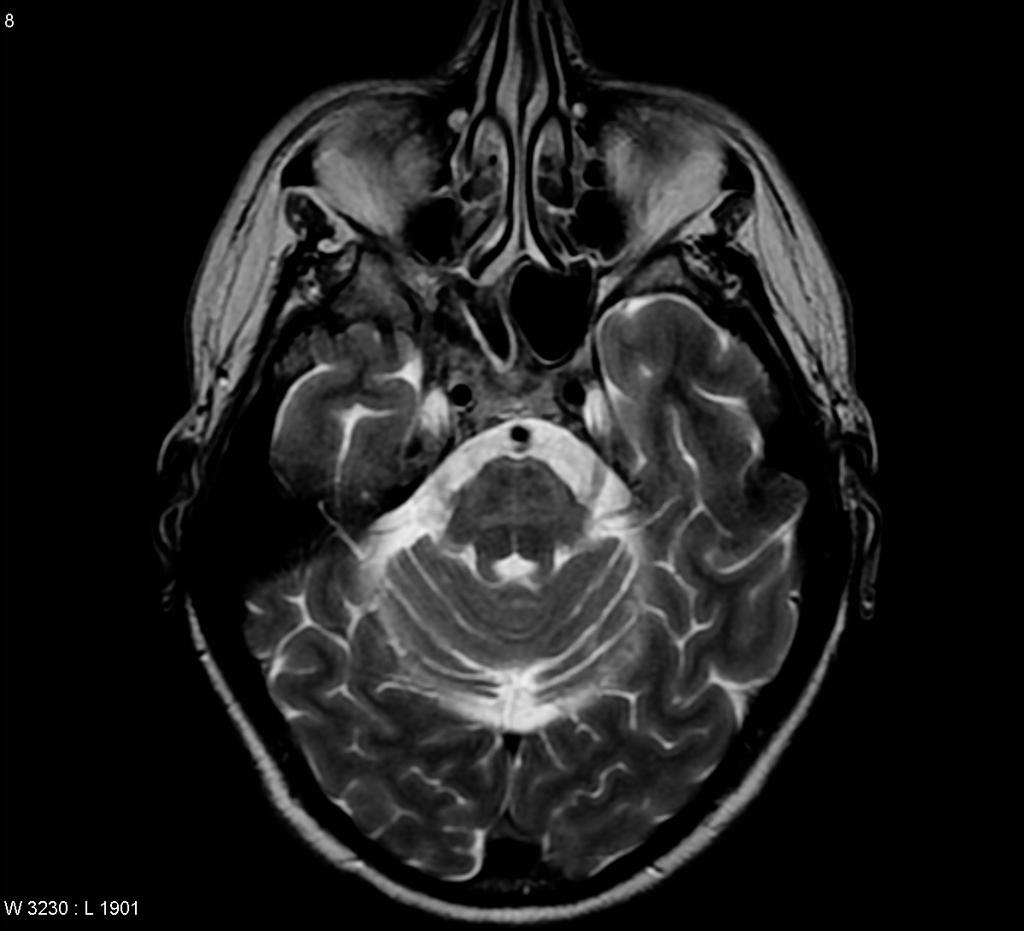
These findings have raised red flags for clinicians and scientists who come into contact with MSA tissue. Many times, doctors mistake signs of MSA for Parkinson’s symptoms. As a result, MSA patients are treated with deep-brain stimulation (DBS), a therapeutic treatment for Parkinson’s disease. The equipment for DBS is made of stainless steel, which prions can easily cling to, and standard disinfection techniques that usually remove microbes do not eliminate the prions that cause CJD. If prions in MSA are similarly resistant to inactivation, MSA could be transmitted when the surgical equipment is reused on another patient.
To prevent the risk of MSA spread, the first precautionary approach is that any equipment that has touched central nervous system tissue should not be reused. Additionally, the World Health Organization (WHO) recommends following its guidelines to sterilize surgical tools. Because prions are resistant to heat, enzymes that degrade proteins, and even radiation, the WHO method of prion decontamination relies on the total destruction of protein structure. Through these precautions, doctors can prevent the spread of the first new prion disease identified in 50 years.
Cover Image: The insertion of an electrode during deep brain simulation — proper cleaning of medical instruments after surgery like this is a key step in preventing the spread of new prion diseases. Image courtesy of Wikimedia.