In 1984, when human immunodeficiency virus (HIV) was discovered as the cause of AIDS, researchers were optimistic that a cure was on the horizon. Now, more than 30 years later, 35 million individuals around the world are infected with HIV. And the cure is still elusive. Why has HIV proven so difficult to treat? The answer lies partly in its ability to remain latent in the human body, staying hidden until it unpredictably reactivates to become deadly once again.
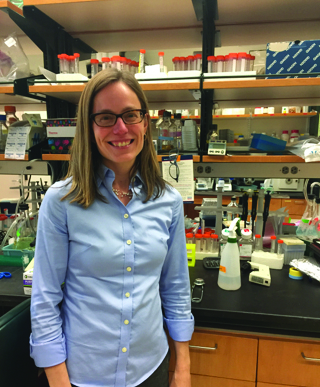
A team at the Yale School of Engineering and Applied Science, led by professor Kathryn Miller-Jensen, is interested in the reactivation of latent HIV. These hidden viruses pose a major hurdle for HIV treatments — even the most potent drugs cannot eliminate the virus until it resurfaces. Current treatments for the disease involve a drug cocktail that patients must take for their entire lives, since latent HIV could reactivate at any time. But what if researchers found a way to force latent HIV back into action in our immune system cells? By drawing these viruses out of hiding, treatments could theoretically destroy nearly all viruses in the body, effectively curing the patient. There is a long road ahead in developing a cure, but projects at Miller-Jensen’s lab might eliminate barriers by illuminating the details of HIV reactivation.
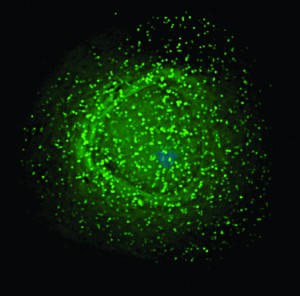
The lab has several ongoing projects working to address the mystery. The team is investigating, for example, how T-cells in the human immune system respond to HIV infection. When HIV invades a T-cell, it inserts its genome into the host genome. Most of the time, the host cell transcribes the HIV genome, the first step to gene expression that then produces more viruses. However, in some cases, HIV instead enters a latent state where it is hidden in the host genome until changes in the T-cells cause reactivation. As such, the lethal virus remains tucked away in a small percentage of the body’s cells.
What kinds of changes to host cells predict reactivation? A component of Miller-Jensen’s research examines latency-reversing agents (LRAs), or small proteins that stimulate HIV back into action.
LRAs can be manufactured into small molecule drugs, which could prove useful in HIV treatments — namely, in the “shock and kill” method. This approach to combatting HIV forces reactivation from the latent state, making all viruses in the body vulnerable to drug action. Other medications then work to eliminate infected cells.
“If we could get all the latent HIV to reactivate, that would allow us to flush out the virus,” Miller-Jensen said. “Basically, there are two parts to the method: First, LRAs are used to reactivate the HIV, and then the immune system or the replicating virus kills off the cells that are now producing HIV.”
Still, like so many promising solutions in science, the “shock and kill” technique has its limitations. Sometimes, significant levels of latent HIV remain in cells even after drugging with LRAs. One possible reason for this is that fluctuations in the levels of gene transcription between cells can cause some cells to respond less strongly to the drugs. “Even if our cells are genetically identical, they don’t always respond the same way,” Miller-Jensen said. “That’s a very interesting question in the field of HIV.”
The group is further is interested in discovering the markers that differentiate infected from uninfected T-cells, which would facilitate identification of cells that are carrying latent HIV. Once again, this could inform more successful therapies for the disease.
Is a cure for HIV a possibility in the near future, or are we still as naïve as in 1984? Will an effective cure remain out of reach despite our improved understanding of the disease? Miller-Jensen is realistic. She does not claim that a cure will be developed anytime soon. “It feels like we’re still pretty far from this goal,” she said.
However, she believes that researchers will continue to make progress by collaborating across fields. “We’re much closer than we were 10 years ago. With many researchers working on different aspects of the problem — finding new LRAs, mobilizing the immune system to kill reactivated T-cells, developing new methods to track the size of the latent reservoir — we might get some kind of combination which solves the problem,” she said.