Growing up, you probably heard council from your parents to put on a coat to avoid catching a cold. Or perhaps you regularly caught some sniffles during the long winter months. As you aged and matured, you might have started to think of “the cold” as nothing more than an old wives’ tale. As a Yale research team recently found out, your parents may have been right.
Led by Dr. Ellen Foxman, a physician in the Department of Laboratory Medicine and a research fellow in Akiko Iwasaki’s laboratory at Yale, the team of scientists determined that key components of the immune system are less able to defend against rhinovirus infections at lower temperatures. Rhinovirus is the most common cause of what we popularly refer to as “the cold,” and it was injected by Foxman and her colleagues into mouse airway cells. These cell cultures were kept at either 33 or 37 degrees Celsius. Foxman found that cells kept at the colder temperature produced far fewer innate immune signals to guard against the viral infection. In other words, the cold made cells more vulnerable to rhinovirus.

This difference in immune signaling resulted in a 100- to 1,000-fold amplification of viral replication at the colder temperature. “A very small environmental change like temperature can make a huge difference in the immune response to an infection and the outcome,” Foxman said.
Ever since rhinoviruses were first cultured, scientists have known that they are better at infecting cells at temperatures lower than our core body temperature. Up until now, however, no one was quite sure why. Why are we more likely to get sick in the winter, when temperatures become frigid? What is it about the cold that gives rhinovirus a competitive edge against the immune system?
Prior researchers had isolated individual events in the viral replication cycle, including cell entry and RNA replication, to investigate this question. Temperature made little to no difference in the efficiency of independent viral processes. Foxman and Iwasaki’s team was more focused on the details of the immune response to the virus rather than the virus itself. Foxman’s investigations into innate antiviral systems led to this study. “My goal at first was to use genetic knockout mice to identify which parts of the immune system are needed to fight rhinovirus,” Foxman said. Knocking out genes systematically would eliminate specific immune functions, allowing her to determine the most critical steps in immune response.

Foxman’s investigation into the temperature dependence of the antiviral response came later. “At the beginning, I was trying to identify which parts of the immune system are needed to fight the virus, but I didn’t know which temperature I should use to do the study,” she said.
The Yale team generated a mouse-adapted strain of rhinovirus through serial passage, a process of repeatedly infecting a mouse with rhinovirus and using viruses produced by that infection to infect other mice. Collaborating with Paul Turner’s laboratory in ecology and evolutionary biology, the researchers found that a majority of the viral proteins found in the mice contained mutations that elicited an immune response. Under normal conditions, sensor-like proteins of the immune system detect the unusual RNA strands of rhinovirus, stimulating the production of signaling proteins called interferons. Interferon signaling helps cells fight viral infection — but as Foxman observed, this process is inhibited at low temperatures. A dip in interferon protection enables rhinovirus to escape an immune attack.
When the team found that interferon production was significantly higher at 37 degrees, they realized they were on the edge of something big. To test whether this difference in immune response also made a difference in the success of rhinovirus infection, Foxman infected cells of knockout mice that lacked key components of the interferon-signaling pathway. She found that the virus replicated much more efficiently at the higher temperature when innate immune genes were missing. Surprisingly, even in the cells from knockout mice, viral production was slightly greater at the cooler temperature. Foxman believes these results might mean that there are other temperature-dependent mechanisms that our bodies utilize in fighting rhinovirus infections. She hopes that future research will elucidate some of these other mechanisms.
For Foxman, one of the most exciting implications of this discovery is that small environmental changes can in fact have a big impact on the outcome of infections to the human body. “If we can understand some things that can shift the balance of the immune response, we can control viral infections,” Foxman said. As a result of her team’s work, investigators may have at their disposal new tools for controlling infections and for manipulating the immune response.
And Foxman does not want to stop there — she hopes that further research into these topics of the immune system will continue to yield new discoveries. “There must be other things we don’t know about that modulate our immune response, and if we could just identify them, we can shift the balance in our favor,” she said.
In particular, Foxman is interested in why viral infections cause different symptoms in different people. At any given time, 20 percent of adults have rhinovirus in their noses, and only some of these infections manifest in cold symptoms.
Foxman’s research tells us that our chance of falling prey to disease does not rely solely on the things that infect us, but perhaps more so on our own day-to-day choices: Should you wear an extra layer today? Is it really a good idea to impress your friends by going outside in your Speedo to make that snow angel? Beyond personal health implications, Foxman and Iwasaki’s work reveals potential new ways of controlling the immune system for research and medical purposes. Additionally, the commercial world is beginning to take notice of this Yale team’s work as contractors think about what temperature dependence could mean for product sales.
“I’ve had sauna manufacturers call me to ask whether they can market their saunas as medically therapeutic,” Iwasaki said. So bundle up and stay warm!
About the Author: Zach is a senior molecular biophysics and biochemistry major in Davenport College. He studies natural product inhibitors of Human Papilloma Virus cell entry in the Iwasaki Laboratory.
Further Reading:
Ellen Foxman, James Storer, Megan Fitzgerald, Bethany Wasik, Lin Hou, Hongyu Zhao, Paul Turner, Anna Marie Pyle, Akiko Iwasaki. “Temperature-dependent Innate Defense Against the Common Cold Virus Limits Viral Replication at Warm Temperature in Mouse Airway Cells.” PNAS 112 (3): 827-832. doi: 10.1073/pnas.1411030112
Beth Mole. “Cold Viruses Thrive in Frosty Conditions.” Nature (May 2013): Online Article. doi: 10.1038.
Peter Wark, Sebastian Johnston, Fabio Bucchieri, Robert Powell, Sarah Puddicombe, Vasile Laza-Stanca, Stephen Holgate, Donna Davis. “Athsmatic Bronchial Epithelial Cells have a Deficient Innate Immune Response to Infection with Rhinovirus.” J Exp Med 201 (6): 937-947. Doi: 10.1064/jem.20041901
Ellen Foxman. “Catching a Cold.” Online Video. Vimeo.
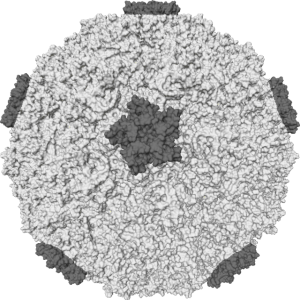
Cover Image: Art by Emma Healy
Acknowledgments: The author would like to thank Dr. Ellen Foxman for her time and her enthusiasm about immunobiology and her research.
