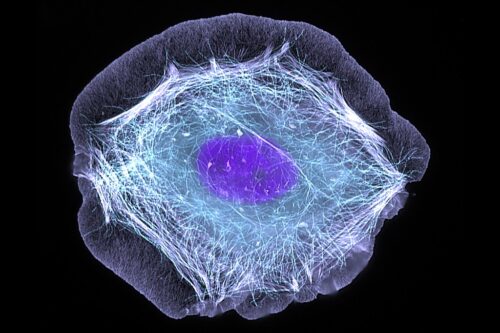
CD8 T cells—a specialized type of white blood cell—play a central role in resisting viral infection. The body responds to various disorders by producing highly functional “flavors” of T cells. Effectors are short-lived, but actively destroy infected and cancerous cells. On the contrary, memory T cells endure long after an infection is cured, enabling a rapid response to that pathogen in the future. Vaccines function precisely by triggering the creation of these T cells, along with B cell-derived antibodies.
And yet, as in any prolonged battle, the “frontline soldiers” of our body’s defenses can get worn out. In cases of acute infection that are quickly resolved, T cells develop predictably and linearly into functional states. But in chronic cases, they develop into dysfunctional states, enabling the infection or cancer to persist.
A recent paper by the Joshi Lab at Yale’s Department of Immunobiology explores the factors behind this phenomenon of T cell exhaustion. They discovered that KLF2—a type of protein that regulates DNA-RNA transcription, and is therefore referred to as a transcription factor—plays a crucial role in modulating the developmental trajectory of effector T cells, and stifling divergence toward exhausted states. Moreover, they observed that KLF2 acts as a “master” regulator; it enables other transcription factors to function correctly.
The study’s first step involved infecting mice models with either acute or chronic strains of lymphocytic choriomeningitis. Then, to evaluate the relative role of thirty-nine transcription factors and epigenetic modifiers, the scientists utilized Perturb-SEQ: a technique that integrates gene-editing technology with single-cell RNA sequencing.By cutting out specific sections of T cells’ DNA with a technology known as CRISPR, they observed the consequences of “knocking out” each gene. “There are fifty thousand cells here, and each cell has a unique knockout,” said Eric Fagerberg (GSAS ’25), a doctoral student and the study’s lead author. “And so we get a ton of info for each gene.”
However, when studying such a heterogeneous population, the researchers had to record this data incredibly precisely to distinguish individual variation at a cellular level. That’s where the second part of Perturb-SEQ came into play. “Biologists look at RNA as a surrogate for the protein,” Fagerberg said. Hence, RNA sequencing is a popular way to study what a group of cells expresses. “But single-cell RNA enables us to do that on a cell-by-cell basis, and capture the heterogeneity of a population in any given context.”
Given this data, the scientists were able to map the trajectory of each gene-edited T cell. This revealed the crucial role of one specific protein. “If we knock out KLF2, we observe that they enrich, quite strongly, in the dysfunctional part of the map unique to chronic infection,” Fagerberg said. If KLF2 is removed, an acute infection takes on features of a chronic one. The linear trajectory that typifies the body’s response to acute infection is disrupted, as T cells enter unexpected, dysfunctional states.
This surprising discovery has a dual explanation. Firstly, KLF2 suppresses TOX, the transcription factor that drives T cell exhaustion. To give evidence for this hypothesis, the team over-expressed KLF2 in T cells with and without KLF2 knocked out that were responding to acute infection. T cells without KLF2 started with a disproportionately high level of TOX. Yet, when the scientists over-expressed KLF2, the TOX gene was reduced to its natural state. They also observed a similar reduction in TOX in the context of chronic infection.
KLF2 also supports the function of TBET, a transcription factor crucial to the production of effector T cells. The researchers tested this by overexpressing TBET in T cells with and without KLF2 knocked out. Although effector differentiation markers were heightened in the cells with KLF2, there was no significant change in those with KLF2 deactivated. “KLF2 likely regulates the epigenetic state—how ‘open’ or ‘closed’ the DNA is—and it may regulate openings where TBET exerts function,” Fagerberg said.
Hence, KLF2 enables T cells to develop along functional trajectories and guards against undesirable states of exhaustion. This discovery opens a door for future exploration about the relationships between KLF2 and other transcription factors, such as TBET, that are dependent on KLF2. Moreover, investigating other cells in immune response pathways (such as CD4 helper cells to CD8 T cells) may reveal further dependencies and ways to enhance the body’s defenses. Fagerberg’s research, by identifying a key factor for safeguarding T cell function, is likely to inspire advances in cancer care, immunotherapy, and more.