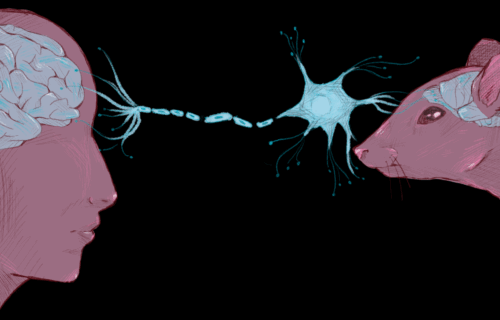
Art by Melody Jiang
Neurodegenerative disease is the ultimate scourge—it steals our loved ones away by eroding both their minds and bodies. As the global population grows older, complex age-related disorders like neurodegenerative disease are becoming more prevalent, posing a formidable challenge to modern medicine. For most of human history, a diagnosis like Alzheimer’s or Parkinson’s disease was a death sentence; by the time an individual began exhibiting symptoms, it was often too late for meaningful intervention. Today, while a handful of treatments can ease symptoms or moderately slow progression, none can halt the disease at its root—at least not yet.
In a recent study published in Biology, a team based at Yale and UC Davis has developed a new platform that allows researchers to study potential treatments with greater biological accuracy and precision than ever before. By transplanting human neurons into the brains of rodents and nonhuman primates, they established a living model of Huntington’s disease that can examine how emerging treatments interact with diseased neurons in real time.
At the cellular level, neurodegenerative diseases are characterized by the progressive loss of neurons, specialized cells responsible for processing and transmitting information in the brain. The most common form, Alzheimer’s disease, damages neurons in the hippocampus, the brain’s memory hub, and the cerebral cortex, which governs language, reasoning, and other higher-order cognitive functions. As the damage spreads, the brain physically deteriorates, leading to memory loss, cognitive decline, and, ultimately, death.
Huntington’s disease is a rare, inherited neurodegenerative disease that affects about five to ten out of every hundred thousand people in the United States. It is caused by a mutation in the huntingtin gene, which produces a misfolded protein, mutant huntingtin (mHTT). In turn, this misfolded protein causes further problems in protein synthesis and neuronal function in the striatum of the basal ganglia, a brain region primarily responsible for movement control. As the disease progresses, patients develop involuntary jerking or writhing movements known as chorea. Symptoms typically appear in a person’s thirties or forties, but patients don’t typically live more than fifteen years after the initial onset. The disease currently has no cure.
Huntington’s disease eventually kills cells that produce a chemical called gamma-aminobutyric acid (GABA) in the basal ganglia. Ordinarily, GABA prevents neurons from firing out of control. This helps control the brain’s signals to the rest of the body, like those that force muscles to contract and relax. But as these GABA-producing cells die, neuronal signaling becomes erratic.
Hunting for Treatments
One emerging treatment for neurodegenerative diseases like Huntington’s is neuronal cell replacement therapy. This approach replaces the neurons lost to disease with healthy ones by tapping into advances in stem cell biology. Since it is impossible to harvest neurons from donors and directly transplant them into patients, clinicians instead harvest non-neuronal cells and turn them into transplantable neurons over several steps. Scientists take donor cells—usually from skin or blood—and reprogram them into induced pluripotent stem cells (iPSCs). These special cells are like blank slates, with the power to develop into almost any type of cell in the body. For patients with Huntington’s, researchers direct iPSCs to become GABA-producing neurons (induced GABAergic neurons, or iGABAs) and transplant them into the striatum.
Many research groups are investigating different aspects of this approach, exploring everything from how to generate the most robust iGABAs to how these grafted cells interact with diseased host brains. Dustin Wakeman, a preclinical therapeutic development consultant and adjunct assistant professor at Yale School of Medicine, specializes in stem cell-based therapies for neurological disease. In collaboration with Kyle Fink, an assistant professor at the UC Davis Department of Neurology studying animal models of Huntington’s disease, they recently published the study in Biology demonstrating the long-term engraftment and integration of iGABAs in Huntington’s animal models.
Wakeman and colleagues transplanted iGABAs into the brains of rats, mice, and monkeys, animal models that scientists commonly use to study diseases and their potential treatments. Months later, they analyzed brain tissue and found that the human neurons had survived, matured, and developed long-range connections with the host brain. “We showed that these cells could indeed survive for long periods of time, become the neuronal cell types that we hypothesized were required, and actually send neuronal fibers out, innervating the host brain, which is really important for function,” Wakeman said.
Neurons are extensively interconnected, which is essential for communication between cells and neuronal function. To visualize how transplanted cells integrate into these networks, researchers used fluorescent antibodies to label human-specific nerves and microscopy to trace where graft-derived fibers developed. They found human fiber presence across distant brain regions, indicating not only the survival of the grafts but also their integration into the host brain circuitry.
Another advantage of these cells is their consistency. Because iGABAs are commercially available and can be preserved in freezers, experiments can be repeated across laboratories with the same cell population. “Anyone in the world can buy the same cell,” Wakeman said. This reproducibility is essential for biomedical research, allowing different teams to test therapies on a standardized platform.
Old Mice, New Tricks
While testing the iGABAs, Fink and his colleagues developed a novel animal model—R6/NSG mice. The original R6 mice were established in the 1990s as the animal model for Huntington’s disease—they express the mutant HTT gene and rapidly develop symptoms that mimic the disease. However, because they have a healthy immune system, introducing human cells triggers a strong immune response that hinders graft integration and compromises the animals’ own health.
To address this issue, the Fink Lab introduced the R6 mutation to NSG mice, which are immunodeficient and do not reject human grafts. To their pleasant surprise, the new R6/NSG line not only tolerated the grafts but also lived longer than R6 mice. “[R6] only lives between twelve and fourteen weeks, but when we take the immune system away, the mouse now lives for about fourteen months and is much less severe [in Huntington’s symptoms],” Fink said. The exact reason for this extension of life expectancy is unknown, but the prolonged lifespan allows researchers to observe both slow disease progression and long-term graft behavior.
Pathological Protein Transfer
The researchers also used their animal model to study mHTT as a pathological hallmark of Huntington’s disease. The exact origin of these misfolded proteins in neurodegenerative disorders is still an area of debate, but there is growing evidence that they spread from cell to cell through a process called pathological protein transfer. In this process, misfolded proteins move into healthy cells, where they trigger other proteins to misfold and form toxic aggregates, eventually disrupting normal neuronal function. The prototypical example is “mad cow disease,” where a misfolded protein “infects” other proteins, causing them to misfold too. While neurodegenerative diseases cannot be transmitted between people, pathological proteins can be transmitted from cell to cell.
But could this infection process undermine efforts to graft healthy cells into patients with neurodegenerative disease? “There’s a disease modeling angle: what’s happening to human cells when the huntingtin protein goes into healthy cells?” Wakeman said.
Wakeman and Fink tested this idea, looking to see if diseased host cells could cause the proteins in the transplanted human neurons to misfold. The researchers observed that mHTT transferred from diseased host cells to the transplanted human neurons in mice with Huntington’s, confirming that pathological protein transfer might indeed mitigate the effectiveness of neuron grafting. However, both Wakeman and Fink find it a minor complication. Wakeman reasoned that even if some grafted cells are eventually affected, the transplantation could still potentially provide a patient with several years of improved brain function and quality of life before pathological proteins begin to impact parts of the transplant.
Further Implications in Medical Research
Another issue in neurodegenerative disease research is that animal and human neurons don’t always behave the same way. In classical R6 mice, Huntington’s disease progresses far more aggressively than it does in humans. But now, with human neurons grafted into the brain, researchers can observe how the disease unfolds in real time—directly in human cells. If these grafted neurons receive mHTT and begin to degenerate gradually, they offer a more accurate and informative model of human disease progression.
Additionally, since neurodegenerative diseases are currently irreversible, early intervention is key. “There are always windows of when these therapeutics are the most effective. If cells are going away, try to preserve as much as you can,” Fink said. Engrafted neurons offer a window into early disease changes and may eventually serve as a testing ground for therapies designed to halt degeneration in the early stages or before symptoms emerge.
Fink’s lab is now exploring CRISPR-based therapies to treat genetic neurological conditions. “There [are] lots of cool things happening in the cell transplantation community, combinatorial therapeutics, and genetic disorders,” he said.
Neuronal cell replacement, as either a therapy or a disease model, can also be extended to other neurodegenerative diseases. “You can do this in Alzheimer’s models with tau, in Parkinson’s with α-synuclein—they likely share similar mechanisms. We can use these similar mechanisms to learn things about different diseases,” Wakeman said.
While many questions remain about how pathological proteins cause disease and how to best intervene, Wakeman and Fink’s work offers a vital step toward understanding these diseases and developing therapies against them. With reproducible human neurons and better mouse models, the field is steadily moving forward with more realistic and human-relevant platforms. Perhaps one day, combinatorial therapies can rebuild what’s lost in neurodegenerative diseases—one cell at a time.