Empathy is a central tenet in the framework of compassionate medical care.
But critical questions remain: How do doctors achieve empathy? Where does this unresolved empathy originate, and how can we maximize it?
When doctors are emotionally connected to their patients, there are fewer reported medical errors and better overall patient outcomes. This fact led researchers at the Yale Thinking Lab to ask: What data about a patient’s condition will elicit the greatest emotional response? A paper recently published in the Proceedings of the National Academy of Sciences, co-authored by psychology graduate student Matthew Lebowitz and Thinking Lab director Woo-kyoung Ahn, explores this question. The paper describes how physicians relate to patients with mental disorders, comparing the role psychosocial information such as background and upbringing to the role of biological information such as genetic factors. Lebowitz and Ahn concluded that psychosocial data about patients results in a more powerful emotional response from clinicians than does biological data.
The implications of this finding hold tremendous importance, especially considering the movement in the scientific and medical communities away from a purely psychosocial discussion of mental disorders. Over the past decade, there has been a shift in the causal explanation of psychiatric conditions. Scientists now rely more on biological reasoning, focusing on the interplay of genetics and hormone levels to understand how the brain functions and reacts to triggers. Lebowitz explained that when grounded in biology, psychiatric symptoms suffer from a sort of mechanistic dehumanization. Clinicians feel less empathetic toward mental illness when it is rooted heavily in biological causes.

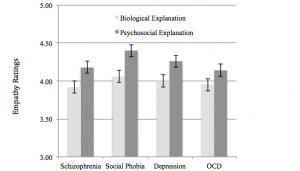
In the first of Lebowitz’s two studies on this topic, clinicians read vignettes depicting patients with either schizophrenia or social phobia. In the second study, patients suffered from either major depression or obsessive-compulsive disorder. The vignettes were categorically divided into biological and psychosocial explanations. The former relied upon genetic and neurobiological factors, while the latter portrayed aspects of a patient’s life history and social setting.
Lebowitz measured empathy by having clinicians read a list of 18 adjectives and rate how they would describe their personal feelings toward the patient in each vignette. He specifically coded the adjectives for empathy, therapeutic reliance, and personal distress. The data revealed that clinicians are inclined to show greater empathy for psychosocial conditions which have an “upsetting or disturbing” nature.
Biological explanations for mental illness can reduce blame, which would lead us to believe that they increase empathy for patients. On the contrary, Lebowitz’s work demonstrates the opposite phenomenon. A possible explanation is that clinicians do not find themselves to be responsible or blameworthy for undesirable circumstances. However, Lebowitz noted that his research did not directly measure blame.
Modern mental clinicians now focus more on the role of genes in diagnosing and treating mental illness and less on traditional cultural and social factors. In this study, participants assessed the extent to which they professionally thought that a patient’s condition could be improved with medication and psychotherapy. A statistical analysis demonstrated that clinicians perceive potential treatment efficacy to be higher when presented with psychosocial vignettes rather than biological vignettes of patient conditions. Thus, this study repeatedly suggests that psychosocial data on a patient’s condition allows for higher treatment efficacy, clinical utility, and overall empathy for the patient.

Lebowitz’s investigation reaffirms the place of psychosocial data in treating those with mental illness. It is important to understand and appreciate the difficulty in unraveling the nuances of empathy toward patients. Lebowitz’s insight into this problem has sparked a dialogue: How should we present a patient’s condition? Should we alter our presentation of the patient’s condition to elicit greater empathy? In the 21st century, with society becoming increasingly concerned over privacy issues, we must not forget that a fundamental understanding of a patient’s background can be a powerful bridge for the therapeutic alliance between mental health provider and patient.
