Exploring the potential control of drug delivery with light and magnetism
Chances are, at some point in your life, you’ve taken some form of medicine in capsule form. In fact, many antibiotics are delivered via ingested capsules. In comparison to tablets—in which the drug forms the tablet itself rather than being contained in a small “shell”—capsules have many advantages, the primary being more efficient drug delivery. Once the capsule is broken or dissolved, the drug it contains is in a form that is faster absorbed into the body.
We are familiar with capsules that are taken orally and dissolve in our stomach, allowing for drug release, but what if these capsules were small enough to be transported in blood vessels to deliver drugs to specific, targeted locations throughout the body? A team at Yale, led by Chinedum Osuji, Associate Professor of Chemical and Environmental Engineering, is designing such capsules. The team has developed a new method of creating tiny capsules, called microcapsules, that respond to light and magnetic cues. Their work may have implications in the ultimate development of controlled, localized drug delivery using microcapsules.
A novel approach to fabrication
A significant component of Osuji’s research is the design of more efficient and simple processes for generating microcapsules. A common microcapsule fabrication method involves a layer-by-layer approach, entailingts sequential steps in which different shell materials are deposited as individual layers onto a template particle. “It’s similar to 3D printing—you just add material layer by layer,” said Gilad Kaufman, a key member of Osuji’s team of researchers. The process, however, is time consuming, and the efficiency with which drugs or other agents are thereafter encapsulated is generally low. These drawbacks have hindered broad adoption of the process.
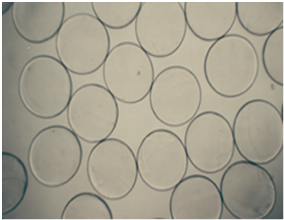
The new microcapsule formation process, designed by Kaufman, Osuji, and Karla Montejo, a summer undergraduate researcher from Florida International University, involves microfluidics—the manipulation of fluid flow on the micro level. There are two key advantages to this process. “One key advantage to microfluidics is that you can very reliably control the size of the droplets and ensure that they are all the same size. You want to have uniform size so that there is little variation in the microcapsule properties—for example, the bioavailability of objects in circulation changes with their size, as does the amount of encapsulated drugs and their release behavior,” Kaufman said. A second important advantage is that the microfluidic approach that they have developed eliminates the need to fabricate multiple layers: the microcapsule shell is formed by creating one relatively thick layer in a single-step rather than many thin ones. This is beneficial in certain scenarios as a thicker shell will result in improved microcapsule mechanical properties, which allows the microcapsules to remain intact and stable until the time of desired release.
Microfluidic capsule “droplets”
Generally, microfluidics can be compared to water flowing through pipes in a house, but with very small pipes. Osuji’s new method of creating microcapsules uses a configuration of “pipes” that facilitates coaxial flow, in which one fluid is surrounded by another fluid. The inside fluid, which contains the drug or substance being encapsulated, is separated into individual droplets as it meets with the outer fluid. Each droplet can be transformed into a microcapsule by interfacial complexation.
Interfacial complexation is not a novel idea. Interfaces are everywhere—they are nothing more than the meeting of two materials. In some cases, interfaces offer you the ability to control reactions. A popular high school experiment looks at the formation of nylon at the interface between two liquids; this nylon can actually be wound up and collected on a spool. More generally, interfacial complexation is when a reaction occurs at the interface of two immiscible liquids, and the solid product of this reaction cannot be dissolved in either of the two liquid reactants. Osuji and his team were the first to use this idea in microfluidic devices to create thick shell microcapsules. In their current research, they performed interfacial complexation using graphene oxide and silicon oil,, thus forming the microcapsule at the interface. The microcapsules that are created in this process can then be used in the desired context.
Finding unique materials
The use of graphene oxide is perhaps one of the key advantages identified in Osuji’s research. An understanding of material interactions is necessary for successful creation of microcapsules via microfluidics. “One of the principle challenges that we had was ensuring the stability of the microcapsule and, of course, the stability of the graphene oxide in the microfluidic device that we used to make the microcapsule,” Osuji said. In other words, a large factor of microcapsule design and formation is making sure that the capsules remain as discrete well-defined objects without spontaneously rupturing, and preventing the capsules from aggregating, or sticking together. Graphene oxide has a high Young’s modulus, which means it is a relatively stiff material, giving the microcapsules a strong shell. Finally, and perhaps most importantly, graphene oxide has photothermal properties, which is key for the photothermal release aspect of the microcapsules.
Photothermal properties have been examined in the context of drug delivery such as cancer therapies for many years now. The concept is simple: upon exposure to light at certain wavelengths, particles can generate cancer-killing heat, or dissociate to release the anti-cancer drug or other therapeutic substance contained inside. Osuji’s new microcapsules have additional benefits. Graphene oxide responds to near-infrared (NIR) and infrared light (IR), a wavelength at which human tissue is almost transparent, meaning that the light can reach the capsule directly without much interference from the human body. “You can envision a system in which you have a capsule carrying some drug and in which the release of the drug can be controlled with light. You can imagine one scenario in which the capsules could be distributed homogenously throughout the body, and another scenario in which you only release the drug where you want—the tumor location, for example,” Osuji said.
Directing the microcapsules
Furthermore, another goal is to not only control the localized release of the drug, but also to direct the capsule to a particular site in the body. To achieve this goal, the team of researchers incorporated ferrite—a form of iron—nanoparticles into the shells of microcapsules by dissolving the ferrite nanoparticles in the liquid of the microfluidic device. With these magnetic ferrite nanoparticles, they were able to direct the microcapsules to specific locations within a vial, and then trigger localized release of the encapsulated substance using NIR light. These experiments confirmed the magnetic response and the NIR-controlled drug release of the microcapsules. That being said, there are limitations to the magnetoresponsive characteristics of the microcapsules.
While the researchers can control capsule movement within a vial in the lab, it is another task entirely to direct the capsules to a certain area of the human body, such as a tumor. In the human body, limitations would likely arise in the ability to direct the magnetic microcapsules due to a complicated blood vessel system and the necessary magnetic field strength—a much stronger magnet would be required to control these microcapsules in the human body. It does show, however, that it’s possible to influence the localization of these capsules on some level. For example, using strong magnets, one can increase the concentration of the capsules in a certain general area of the body, and then control release using light directed at a more concentrated location. In other words, the microcapsules could potentially be magnetically drawn to a given area surrounding a tumor, and the NIR-signaled drug release could be limited to only the specific location of the tumor.
There are further limitations to the biomedical use of these microcapsules. Predominantly, to be used in the body, the capsules must be much smaller than the capsules that Osuji, Kaufman, and their team have been able to create. Currently, Osuji’s capsules are approximately 80 microns in diameter, or about the diameter of a single human hair. “The size of the microcapsule is controlled by various parameters, one of which being the size of the nozzle in the microfluidic device. To be used in blood vessels, the microcapsules should have a diameter of about one micron or smaller. It is much harder to make a nozzle that is sufficiently small to produce microcapsules of that size,” Kaufman said. Furthermore, the size of the droplets is controlled by the intrinsic properties of the fluids themselves, such as surface tension. If you imagine a faucet with dripping water, the sizes of those water droplets are correlated to the rate of water flow, the diameter of the pipe, and the properties of the water.
Looking forward, the new one-step method to create these new photoresponsive and magnetoresponsive microcapsules has many possible biomedical implications. The challenge now is to find a way to shrink these microcapsules, while maintaining their functional and structural integrity, for a direct medical use. “The main difficulty was finding a way to make microcapsules in a simple process that has the potential to be scalable, and also has potential applications by using building blocks that are responsive to specific environmental stimulants,” Kaufman said. Perhaps equally important, the research shows the scientific and medical implications that arise from a combination of very simple ideas. “The idea came and the expertise was there to enact it. It is inherently a simple and versatile process. It is a very accessible technology,” Osuji concluded.