How researchers are demystifying complex lung diseases using models
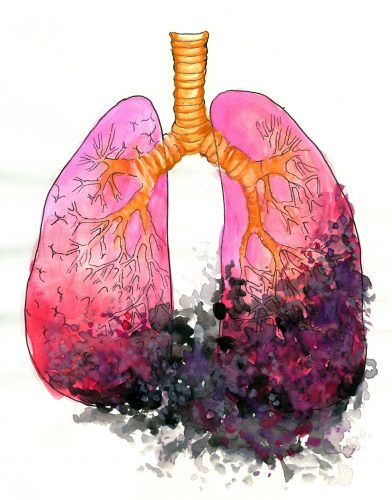
It’s a diagnosis that stumps even the best of doctors. Idiopathic pulmonary fibrosis begins with a small cough and progresses over time to stop lung function—so much so, that patients cannot receive enough oxygen by inhaling. Scarred lung tissue—fibrosis— hardens the lung and makes it difficult to breathe and receive oxygen.
On average, patients can only expect to live two to five years after a diagnosis of idiopathic pulmonary fibrosis (IPF). What’s worse is that doctors come to diagnose IPF only after patients do not respond to any other known treatments for fibrosis. “Idiopathic” means of an unknown cause. Doctors can only scratch their heads in vain, as there is no cure, and no known cause for IPF.
“It really is a disease where we don’t understand why or how it occurs,” said Biomedical Engineering professor Anjelica Gonzalez. “The result is either they die after diagnosis or have a transplant.” But transplants also can result in problems if transplant organs are not compatible with the patient, causing a strong immune response in the patient.
In a collaboration between the Anjelica Gonzalez lab in the Department of Biomedical Engineering and the Erica Herzog lab at the Yale School of Medicine, researchers have been able to engineer human lung tissue and model the process of fibrosis in human lungs. This advancement will make it much easier for researchers to further investigate fibrosis and the effect potential drugs.
Pericytes: The Link in the System
Your blood vessels are like the irrigation system of the body, bringing nutrients and oxygen to the brain, heart, and other specialized cells. Blood vessels vary in size and function; the body’s smallest blood vessels, for example, allow for direct cell-to-blood exchange of nutrients and wastes.
Pericytes are small cells that wrap around the lining of the blood vessels, thereby regulating both blood vessel development and blood flow. Gonzalez has always been interested in the engineering principles behind how blood vessels deliver oxygen to tissues on such a small scale, and began studying the role of pericytes in supporting the circulatory system.
The researchers found a novel role for pericytes in IPF progression. During IPF, tissues die because of limited nutrient and oxygen delivery. Blood vessels in the lungs become disrupted and stop functioning. Pericytes were previously thought to die along with normal tissue cells. But Gonzalez’s lab found that pericytes were not only alive in IPF patients, but they also made up part of origin sites of fibrosis. In other words, the pericytes themselves had become dysfunctional.
Modeling the Lung
With this newfound knowledge of the role of pericytes in fibrosis, Gonzalez’s lab began to engineer human lung tissue that could model the transformation from healthy tissue into stiff fibrotic tissue.
“[The engineered lung] is the size of a thumbnail, a little glass slide that mimics the lung environment,” said Parid Sava, a previous graduate student in the Gonzalez lab and first author on the paper. “We take the scaffolding and match it to the mechanical properties of fibrotic or healthy tissue.”
The scaffolding serves as the base “membrane” upon which cells are anchored. This membrane can be made either stiffer or softer using hydrogels—stiffer scaffolding imitates hardened, scarred fibrotic tissue, while softer scaffolding imitates healthy tissue. Then, the researchers added cells to the scaffolding and observed the outcomes.
Fibrosis is a vicious cycle; the stiffer the original lung tissue is, the more fibrosis that will occur. Researchers identified a compound, transforming growth factor-beta 1 (TGF-β1), that drives pericytes to leave the blood vessels and increase their secretion of proteins that form supporting extracellular matrix, which increases the stiffness of the surrounding tissue. An increase in model tissue stiffness was seen to cause increased fibrosis induction by the pericytes, showing that tissue stiffness can have effects on the severity of fibrosis and the progression of IPF
This modeling technique represents an advancement in research methods, making it easier for researchers to study in human lung fibrosis. Prior to Gonzalez’s research, animal models such as mice were primarily used to study tissue fibrosis. The problem was that animal models repair themselves over time, so animal models cannot be used reliably to model human pulmonary fibrosis progression.
“Lung fibrosis is so extreme because lungs cannot regenerate,” Gonzalez said. For instance, the liver can heal scarred tissue and therefore reduce the damage that liver fibrotic diseases can have—but the lung cannot do the same.
Using human tissue instead of mouse models or organs with the ability to regenerate paints a more accurate picture of the disease. “It gives clinical researchers a better idea of what happens in the human system,” Gonzalez said.
Bringing Hope to Patients
Now that the researchers have a model for how fibrosis progresses, they hope to investigate how to reverse the process of fibrosis. “IPF is a pretty terrible disease…we wanted to figure out why this is happening and find drugs to prolong their lives,” Sava said. “What we’re really excited about is how to re-treat it.”
In the future, researchers will test potential drug candidates on fibrotic models to see if scarred, fibrotic tissue can be converted back into healthy tissue. Treatment with nintedanib, a currently used antifibrotic agent, reduced the progression of lung remodeling by the pericytes. “We’ve looked at three [drugs] and are on the way to a few more,” Gonzalez said. The lab’s lung models not only provide a more accurate depiction of fibrosis, but they also cut down on costs of clinical trials, as drugs can be proved in the tissue models before being tested on mouse models and in human trials.
The new fibrotic models can also be applied to investigating other diseases. Diseases that share a similar progression from soft tissue to scarred fibrotic tissue can also be modeled by using different types of cells to fill in the scaffolding. “We can take tissues from liver fibrosis, kidney fibrosis, and skin fibrosis, for example, and use the same model as before where we figure out what is driving the condition,” Sava said.
Researchers can also model other diseases that involve changes in the tissue of the lung. “In IPF [lung tissue] gets stiff, but in other lung diseases, the tissue degenerates or becomes soft,” Gonzalez said. Now, researchers can begin to understand the role of mechanics on disease and investigate potential new treatments further.
Researchers in the Gonzalez and Herzog labs are taking an interdisciplinary approach not only to investigate potential new therapies but also to make it easier for researchers to investigate therapies in the future. The new model of tissue fibrosis that the Gonzalez lab has created will facilitate new investigations into the causes of and potential treatments for IPF, similar fibrotic diseases in other tissues, and other lung diseases that involve mechanical tissue changes. In the future, perhaps a drug candidate will emerge able to reverse IPF, providing hope to the patients affected with a once incurable, little-understood disease.