It is well known that trillions of microorganisms populate our guts and perform a multitude of beneficial functions, including digestion. However, new research by Yale scientists suggests that one of the generally harmless bacteria in our microbiome might be the key to unearthing the mechanisms behind antiphospholipid syndrome (APS)––an autoimmune disease that induces our immune cells to mount an attack against our own bodies. APS increases one’s risk for blood clots, pregnancy complications, pulmonary embolisms, heart attacks, hemorrhages, and strokes.
APS is a relatively rare disease with an estimated prevalence of roughly one to five percent among the general population. Women are at a slightly greater risk of developing APS. APS shows few warning signs, but it can be deadly. Until now, doctors knew little of the reason for the development of APS, but a team of Yale researchers led by Martin Alexander Kriegel—associate professor adjunct of Immunology and Medicine (Rheumatology) at the Yale School of Medicine—might have found a possible explanation in our gastrointestinal flora.
The group studied a common human gut bacterium—Roseburia intestinalis (R. intestinalis)— suspected of triggering the onset of APS in genetically prone individuals. They hypothesized that because part of the surface of this bacterium closely resembles that of an APS autoantigen known to stimulate an autoimmune response, the immune system may mistakenly identify and interpret the presence of R. intestinalis as a signal to generate antibodies. These antibodies not only attack the bacteria, but also the phospholipids in our bloodstream and cell membranes, resulting in blood clots and organ damage. The resemblance between the molecules targeted in APS and those found on R. intestinalis led the researchers to investigate how the microbiome contributes to autoimmune disorders.
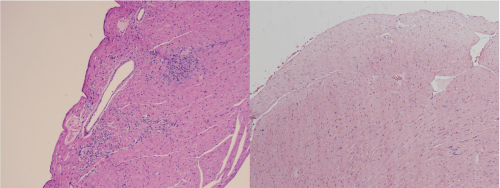
The researchers studied both animal models and human tissues obtained from APS patients. For the animal model, they implanted R. intestinalis into a group of genetically edited mice. In response, the colonized mice exhibited an inflammatory reaction to the autoantigen, as expected for APS. A different group of mice was pre-treated with an antibiotic but not implanted with R. intestinalis. The fact that these mice did not demonstrate the same kind of tissue damage suggests that the R. intestinalis may help promote the development of APS.
In human studies, APS patients had fecal, blood, and plasma samples tested for systemic inflammation markers as well as chemicals that validated antimicrobial responses––particularly antibodies produced by B cells in response to R. intestinalis. The researchers’ findings revealed that rates for those antibodies were more highly elevated in APS patients than in healthy individuals, strengthening the argument that relates cross-reactivity to systemic inflammation.
“This is one of the first studies in humans showing that there is a common gut microbe that can trigger cross-reactive T and B immune cells responses in autoimmune patients,” Kriegel said. “Particularly for antiphospholipid syndrome, [a relationship with] the gut microbiome has not really been studied. We believe we made the first mechanistic link between this devastating disease and the gut microbiome”.
While the findings uncovered by this study were particular to APS, these discoveries could point to analogous pathways for elucidating the mechanisms behind other autoimmune diseases, which may be quite similar in nature.
“There could be many more microbes that act like R. intestinalis because we have so many of them [living inside of us] and even more microbial antigens that could be similar to self-structures, which the immune system mistakes for these microbes and then attacks,” explained Dr. Kriegel. “This is a growing field and there are more findings like that. It speaks to the older paradigm of infectious diseases inducing transient autoimmune diseases, such as rheumatic fever or Guillain-Barré syndrome. These were linked to transient infectious agents that caused cross-reactivity, but with the microbiome, we now have several [identifiable] chronic triggers, which could be the missing pieces in the puzzle of chronic autoimmune diseases,” Kriegel added.
Through their examination of the microbiome’s relationship to APS, the researchers might have taken an important step towards improving our understanding and potential future treatment of autoimmune diseases.