Take a moment to appreciate how powerful your immune system is. Over millions of years, evolution has selected for specimens with the ability to identify an essentially infinite number of foreign objects, or antigens, in our bodies, and develop antibodies to attack them. This is why we are able to survive over 200 types of the common cold.
But with great power, notes Peter Parker’s Uncle Ben, comes great responsibility. To successfully attack our bodies, antigens must be relatively similar to our own cells. Your immune system has to carefully identify which agents in the body are foreign; sometimes, it can be too good. This is the basis of autoimmune disease: when the body misidentifies its own cells as pathogens and attacks them.
“Myasthenia gravis” (MG) literally translates to grave muscle weakness. “For the longest time, it was thought to be like a muscular dystrophy, in that it was chronic, typically progressive and with no available disease-modifying treatment ” said Professor Richard J. Nowak, a physician-scientist, in the Department of Neurology at the Yale School of Medicine. In the 1970s, it was discovered to be an autoimmune disease. This was a “major game changer” said Dr. Nowak.
Take another moment to appreciate your physical body. Each time you take a step or move your eye across a page to read a sentence, you make a decision. Your brain relays that decision to your muscles and induces their compliance. This communication occurs at a neuromuscular junction (NMJ).
The neuron contains neurotransmitters in synaptic vesicles, which are released at the NMJ and make their way to receptors on the surface of the muscle in question. In fact, there are so many of these receptors that the muscle surface is folded up into small villi to accommodate all of them. The neurotransmitter and receptor fit like pieces in a puzzle: something clicks, and the muscle knows to contract or release, causing motion.
In MG, the immune system mistakes one these critical components, the acetylcholine receptor, for a pathogen. B-cells, crucial agents of the immune system, flood the body with autoantibodies, which attach to the acetylcholine receptors on the muscle surface. The receptors no longer can bind the acetylcholine, and the neuromuscular communication fails. Movement becomes difficult and weakness results.
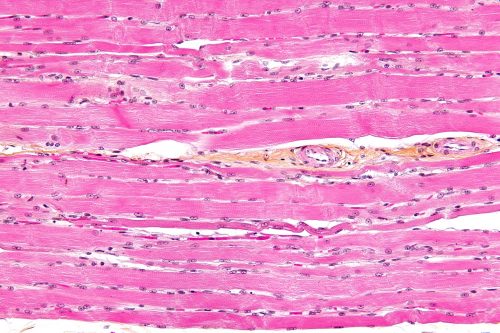
MG has traditionally been treated with immunosuppressants, like steroids. These treatments globally suppress the immune system, resulting in fewer life threatening attacks of the acetylcholine receptors. The sometimes chronic and continuous attack by the autoantibodies eventually takes its toll. “After a long period of active and unchecked autoimmunity, the architecture of the muscle surface is flattened,” said Nowak. The villi close up, leaving ever fewer receptors accessible to the neurotransmitter. “It was not uncommon for patients to die from [MG] in the past, because their respiratory muscles weaken, their diaphragm weakens and they can’t breathe on their own.” Current immunosuppressive strategies are not targeted and can result in significant side effects when used chronically along with the fact that about 15% of patients do not respond to standard treatments.
But what if you could attack only the rogue B-cells, that ones that produce the autoantibodies and remove them completely? Nowak’s group is studying such a drug.
Rituximab was developed about twenty years ago in the treatment of non-Hodgkin’s lymphoma, which is a cancer of B-cells. One unfortunate patient also had MG and showed dramatic improvement in those symptoms. “Rituximab targets the CD20 antigen, which is expressed on B-cells that are antibody producing,” said Nowak. “It is administered intravenously once a week for four weeks.” The cycle is repeated six months later. The clinical benefits show several weeks to months later, so long-term follow-up is key.
Nowak’s team followed a group of 16 patients up to 8 years. After a year, most were able to reduce, or completely stop, their use of other immunosuppressants. The mean time until relapse was three years after treatment was completed. “This is the longest relapse time recorded in any treatment for MG,” remarked Nowak.
Affecting up to 100,000 individuals in the U.S., myasthenia gravis is considered a rare disease and as such there is a paucity of large interventional clinical trials. Many treatments currently in use are based on small studies or anecdotal experience and do not have an FDA-approved indication. Most health insurance companies are resistant to covering these treatments as a result.
Careful studies are necessary to ensure the treatment’s validity, notes Nowak and further explains that “everyone wants a prospective, placebo-controlled trial”. The team has already begun such a trial: BeatMG Study. “We anticipate results in late 2017.”