The process of drug development is enigmatic to most of us. Several groups, labs, and industries contribute considerable time and resources to producing the medicines which keep us healthy. The key to a drug’s success is the interplay between industry, which ultimately produces the drug, and academic research, where the “next big drug” is usually discovered. Research can be a slow and uncertain process–years pass seamlessly between major discoveries. In contrast, the companies that translate these discoveries into the clinic follow a strict, fast-moving timeline.
In rapidly expanding fields of science like cancer immunotherapy, the disconnect between academic research and industry can sometimes lead to problems. A recent study in the Chen group at the Yale School of Medicine has overturned our traditional understanding of a certain immunological mechanism–brining under scrutiny the use of certain drugs which have been used by pharmaceutical industry for years. In the study, the researchers characterized and examined the interaction between fibrinogen-like protein 1 (FGL-1) and the LAG-3 receptor on immune T cells. The results of this study could lead to the development of better treatments in the field of cancer immunotherapy.
The immune system
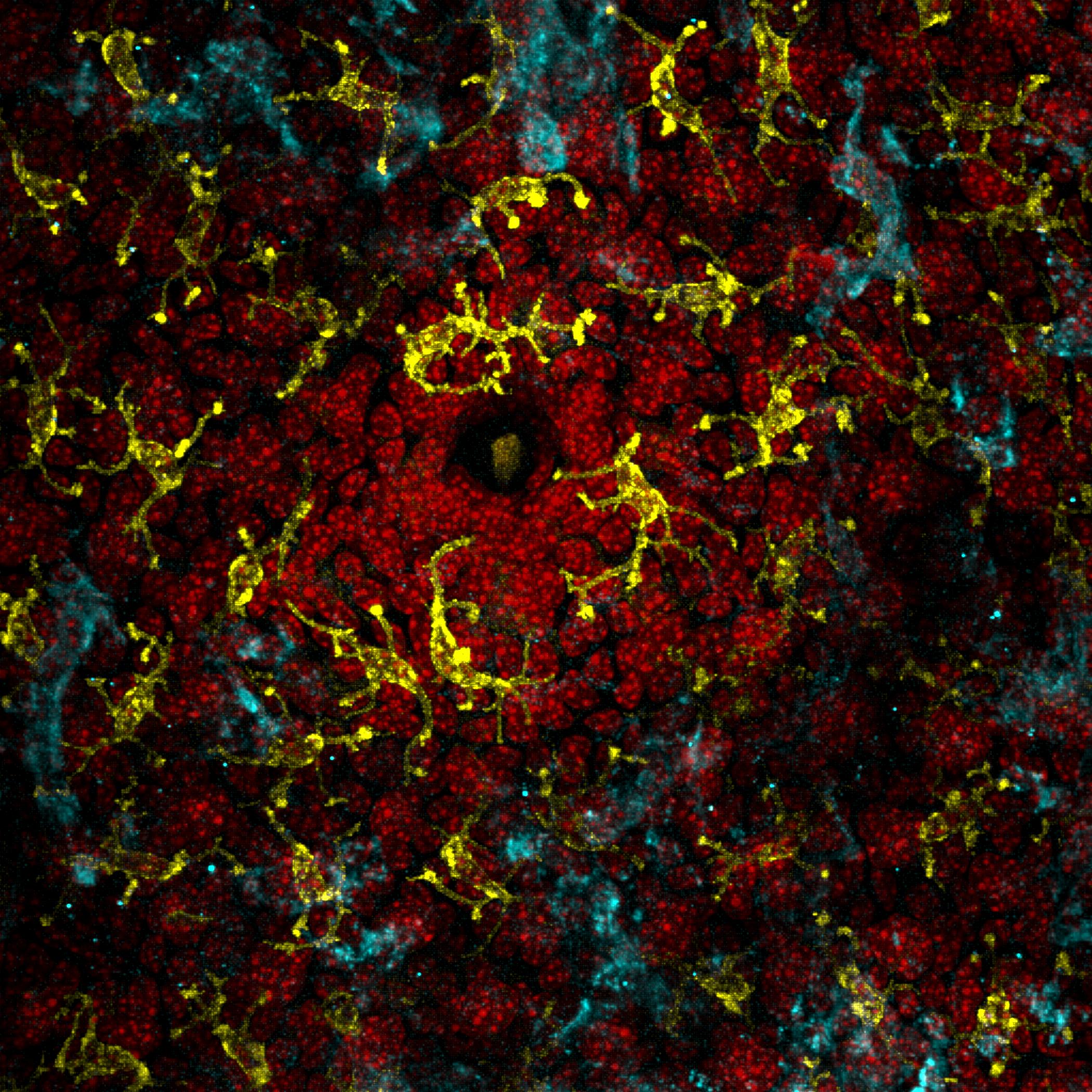
The human immune system is an intricate machine because of the amazing variety of threats it has to recognize and deal with, from bacteria, to viruses, to even fungi. Its operation is centered around innate immunity, which involves recognizing interactions between molecular sensors attached to immune cells and common types of molecules on foreign cells. But some invaders, such as viruses, cannot be recognized in this way. In response, every non-immune human cell has evolved antibodies and the major histocompatibility complex ligands class I or II (MHC I/II), which are attached to the cell surface and serve as a diagnostic tool for immune T cells.
The MHC ligand samples protein fragments from inside the cell and presents it for inspection by the T cells, which roam around like policemen. When a virus invades and forces the cell to produce abnormal proteins, these proteins will appear on the MHC-I, and the T cell responsible for identifying it will be activated. In many cases, the T cell will kill the infected cell and stop widespread infection.
In a pinch, this process also allows T cells to detect and kill cancer cells. Cancer cells originate from accumulated random mutations that endow them with an abnormally high proliferation rate, allowing these cancer cells to grow unchecked in the body. These mutations often result in abnormal protein production, which are sampled and presented on the MHC-I ligand on the cell’s surface. T cells can recognize this abnormality and act as necessary.
What is cancer immunology?
This study was supervised by Lieping Chen, United Technologies Corporation professor in cancer research and professor of Immunobiology, Dermatology, and Medicine at Yale. He had previously revolutionized cancer treatment with his discovery and characterization of the PD-L1 ligand, a cell-death pathway that cancer cells hijack to prevent an immune response. His research group works to use the human body’s natural immune system to fight cancer. To do so, the team faces a number of challenges. Cancer cells proliferate rapidly and can thereby rapidly evolve defenses against T cells. One such defense is misdirection–when binding between an abnormal MHC-I ligand and a T cell receptor sends off an alarm signal, the cancer cell can induce other interactions that cancel out that signal, or even kill the T cell.
For example, a cancer cell under attack by the immune system can evolve the PD-L1 ligand. The next time a T cell binds to the MHC-I, the cancer cell will attach its PD-L1 ligand to the PD-1 receptor on the T cell. This binding sends a signal to the T cell to both stop attacking and to self-terminate through apoptosis. The PD-L1 ligand is, in essence, the cancer cell’s “get out of jail free” card.
To mitigate the cancer cell’s defenses, cancer immunologists can introduce antibodies that block the T cell’s PD-1 receptor. The T cell regains the ability to bind to the MHC ligand and sound the alarm. This, of course, prompts the cancer cell line to either find another way to suppress immune cells or die out. What results is a game of cat-and-mouse between the cancer cell and the T cell. Clearly, an understanding of the various interactions between cancer cells and immune system receptors, as well as the cellular responses they induce, is critical to controlling cancer.
Signals of an issue
Another receptor that caught the eye of the Chen group was LAG-3 on T cells. LAG-3, like PD-1, is an inhibitory receptor on T cells. That is, if a suitable molecule binds in a complementary manner to LAG-3, the T cell loses its ability to attack foreign and cancerous cells. Discovered before PD-1, the MHC-II ligand–the version of MHC ligand on specialized immune cells–was commonly thought to be the complementary ligand to the LAG-3 receptor for decades. As a result, numerous pharmaceutical companies produced drugs to block LAG-3 from binding to MHC-II. The rationale was that introducing molecules that crowd out the MHC-II ligands will allow LAG-3 will be unbound, allowing T cells to remain active.
However, evidence had been mounting that MHC-II is not the major ligand that pairs with LAG-3. A number of research studies demonstrated that other kinds of molecules that prevent LAG-3-mediated inactivation without blocking MHC-II were effective at amplifying T-cell responses and managing tumors, indicating that the MHC-II/LAG-3 interaction may not be as important as researchers thought.
Unfortunately, the majority of LAG-3 targeting drugs pushed to clinical trials are still MHC-II blockers. Jun Wang, an associate research scientist in the Chen lab and first author on the paper, is acutely aware of this issue. “This phenomenon has been in this field for more than fifteen years…people know the issue is there, but they don’t know the biology and so they continue to produce MHC-II blockers,” Wang said. It was this widespread issue that drew Wang to investigate. “I got to thinking, ‘maybe MHC-II isn’t the major ligand. Maybe the ligand is somewhere else,” Wang said.
Dispelling an old misunderstanding
Wang began experimenting by growing T cells and cancer cells together in a medium lacking serum, a slurry of the different proteins and fluids typically used to help cells remain healthy in laboratory dishes. In this case, using MHC-II blocking antibodies induced no therapeutic response whatsoever, whereas use of the same antibodies on cells grown on regular serum medium had a small effect on cancer cell growth. This experiment indicated that the antibodies weren’t blocking MHC-II, but rather something in the serum that was responsible for binding to LAG-3.
To find the molecule responsible in the serum, the team scanned the human genome for proteins that would bind to LAG-3. Using what is termed a GSRA assay, they found that fibrinogen-like protein 1 (FGL-1), a protein normally produced in the liver, had a very high binding affinity for LAG-3. “We generate antibodies as therapeutic drugs because they have very high affinity for receptors…but [the FGL-1/LAG-3 interaction] has a very high affinity, just like on the antibody level,” Wang said.
Further experimentation confirmed the importance of this interaction towards cancer research. A biophysical study found that FGL-1 binds to the area of LAG-3 that is blocked by the non-MHC-II blockers often used in laboratory studies, finally explaining the effectiveness of these blockers in years of studies. Furthermore, knocking out the FGL-1 gene reduced T cell deactivation at a comparable level to LAG-3, further strengthening the connection between the two. Finally, just like PD-L1, the team found that FGL-1 was greatly upregulated in humans with solid tumor cancers, indicating that the protein acts as a defensive measure used by cancer cells against T cells and could serve as a helpful biomarker for cancer immunotherapy.
This research demonstrates that FGL-1 is the complementary ligand to LAG-3, meaning that the numerous drugs produced to target MHC-II are relying on biological assumptions proven to be false. Chen hopes that his team’s research will lead to the creation of new treatments which take advantage of this newly discovered FGL-1/LAG-3 interaction.