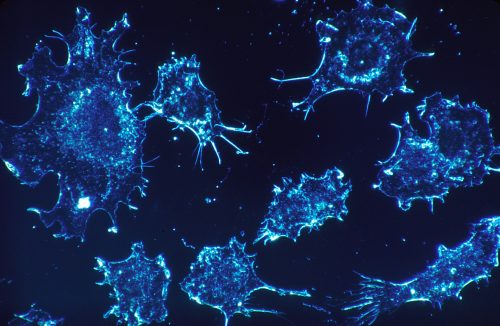
Cancer is estimated to affect forty percent of individuals in the United States at some point in their lifetimes. Cancer is marked by rapid, unchecked cell growth and proliferation, which has led researchers to investigate and refine cytotoxic, or cell-killing, treatments. However, with over one hundred forms of cancer, many traditional cytotoxic methods have only had moderate success.
A recent development in cancer therapy involves genetically engineered T-cells that are removed, modified, and re-injected into the patient to enhance their ability to attack a specific antigen expressed by cancer cells. One of these engineered T-cells are called chimeric antigen receptor (CAR) T-cells. While this strategy has proven effective in early stages of clinical trials in patients with lymphomas, patient response to the treatment remains unpredictable due to our limited knowledge of the CAR-T cells’ immune responses when they encounter cancer cells at the systems level once they have been re-injected into the patient.
A Yale research team led by Rong Fan, an associate professor of biomedical engineering, has made critical findings regarding the CAR-T cell activation pathway. Using high throughput sequencing and single-cell analytical techniques, Fan’s team determined that CAR T-cells toxicity to tumorous cells is mediated by a group of proteins called cytokines, which are cell signaling molecules responsible for growth, proliferation, differentiation, and other functions mediating the mechanism of action to battle cancer cells once CAR-T cells are activated.
Researchers found that a subtype of white blood cells, called CD4 + helper T cells—which are usually regarded as a group of T cells specialized in assisting other immune cells to battle pathogens or cancer cells rather than directly killing infected or cancerous cells like CD8 cytotoxic T cells—are as effective as CD8 cells in directly killing tumor cells. Moreover, CD4+ cells produce similar cytokines if they are engineered to express CAR. Furthermore, Fan’s lab found that CD4+ CAR-T cells differ substantially from classical T cells in that they do not conform into one of the major subtypes, but exhibit a hybrid state combining the function of both Th1 and Th2, making these engineered T cells much more powerful and multifunctional. Usually, a T cell needs to differentiate from the naïve state all the way to the effector state in order to be ready to fight cancer cells. They found what these CAR-T cells can do are largely independent of their differentiation status, which is another surprising observation. These findings led the lab to propose a model by which CAR-T cells become activated upon interacting with cancer cells to provide a wide range of cytokines independent of the differentiation state.
While elucidating many details about CAR-T cell interactions with cancer cells, the research team did note several areas in which more research is required. Firstly, the unique role of CD4+ CAR-T cells in cancer therapy is still largely unknown. Second, researchers identified one pro-inflammatory cytokine that was surprisingly prevalent in CAR-T cells and may be linked to immune-mediated adverse effects. Despite these areas requiring further research, the methodology designed by the Fan lab can be applied to verifying proper manufacturing of the CAR engineered T cells for treating patients. Further, their results provide critical insight into CAR T-cells, their activation, and their interaction with target molecules. Ultimately, these discoveries can inform and help advance CAR-T targeted therapeutics.