Cancer is the second-largest killer in America and one of the most difficult diseases to treat. How do we possibly target cancer cells when they appear almost exactly the same as our own healthy cells? Recently, two Yale research groups have developed a new therapy that specifically shrinks or kills cancers in mice and can potentially be applied to future treatment in humans.
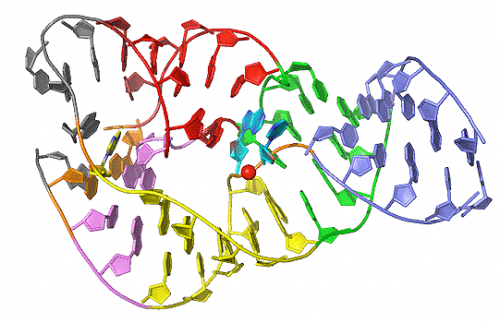
Pursued by the Pyle lab and the Iwasaki lab, the research team designed and synthesized a unique RNA called Stem-Loop RNA 14 (SLR14). SLR14 specifically binds to RIG-I, an important pattern recognition receptor (PRR) located inside the cell that recognizes viral double-stranded RNA. In this model, SLR14 can mimic viral infection in the cell to activate the RIG-I pathway, leading to tumor cell apoptosis or immune system activation to kill tumors.
“Targeting PRRs to treat cancer has been studied for many years,” said Xiaodong Jiang, one of the head researchers of the project from the Iwasaki lab. “Compared with other PRR agonists, there are relatively few studies on RIG-I agonists in cancer treatment. One important question is how to design RNA or agonists that can specifically bind and activate RIG-I, and how to precisely deliver them into the tumor.” As of now, the research group has used an in vivo delivery system, where SLR14 (RNA) is directly delivered to the tumor, and has observed favorable tumor responses and regressions in mice.
“Our aim is to activate the innate sensor pathway within the tumor microenvironment to induce a potent antitumor response,” Jiang explained. “By mimicking virus infection in tumors, SLR14 binds to RIG-I and activates the downstream signals to induce type I interferons (IFNa and IFNb). Through this strategy, we can directly induce tumor cell death, or indirectly kill tumors by inducing immunogenic cell death.” But how does SLR14 avoid killing healthy cells along with the tumors? Previous research demonstrated that normal cells express higher level of anti-apoptotic signals than tumor cells, which allow them to stay healthy and survive.
SLR14 also appeared able to enhance the effectiveness of existing cancer therapies. Tumors can block off the cytotoxic function of surrounding T cells through PD-L1 (on tumor cells) binding to PD-1 (on T cells). Blocking PD-1 or PD-L1 with antibodies, or immune checkpoint blockade therapy, has shown remarkable success in some types of cancer patients. In this study, SLR14 has been observed to improve the antitumor efficacy of anti-PD1; in some cases, it also showed good efficacy in anti-PD1 resistant tumors. In addition, SLR14 activates the T cell response to kill tumor cells by recognizing antigens specifically expressed in tumor cells but not healthy cells.
The research team found success in several types of mouse tumor models, including mouse melanoma and colon cancer. More research is still needed, however, before the treatment is ready to be applied to human patients. Jiang and the rest of the researchers are excited for the future goals of the project: “First, we aim to optimize the delivery system, looking at aspects such as dosage and how to apply RNA intravenously. Second, we want to test in other models such as breast and lung cancer,” Jiang said. Once these pre-clinical models are finished, the ultimate goal is to perform clinical trials and move forward with the studies in human tumors.
This project spreads over several interdisciplinary subject areas, specifically RNA biology and immunology. “Anna Pyle is an expert in RNA. [Her lab] focuses on the structure of RNA. Akiko Iwasaki is a well-known immunologist, specializing in antiviral immunology. I want to emphasize that this has been a very good team work, and we are having a very successful collaboration,” Jiang emphasized. By bringing together experts in RNA biology and immunology, a previously known anti-tumor mechanism has been improved and identified as a promising therapy for treating cancer.