Illustration courtesy of Mila Colizza.
Biological tissue is extraordinarily complex and diverse. Human skin, for example, guards the muscles, bones, and internal organs, protects the body from pathogens, and prevents water loss. Furthermore, skin is composed of a variety of cell types, varies in thickness throughout your body, and is vascularized, or houses blood vessels. Developing new biomedical devices to promote regeneration and healing of our skin tissue is one of the forefronts of current medical research.
The Growth of Tissue Engineering
No matter your interests, you’ve likely encountered tissue engineering in one form or another. Cell culturing, nanofibers, computer aided design, and bioartificial organs are all used in the field known as “regenerative medicine,” a term used synonymously with tissue engineering. According to the National Science Foundation, the origins of tissue engineering can be traced back to the late twentieth century. Since then, the field has experienced unprecedented growth, the volume of research in the area growing throughout the 1990’s and early twenty-first century.
At Yale University, the bulk of tissue engineering research has emerged from the biomedical engineering department, founded in 2003 by W. Mark Saltzman, Goizueta Foundation Professor of Biomedical and Chemical Engineering. Saltzman, in collaboration with Jordan Pober, Bayer Professor of Translational Medicine and Professor of Immunobiology, and Pankaj Karande, Professor of Chemical and Biological Engineering at the Rensselaer Polytechnic Institute (RPI), recently published a paper in Tissue Engineering in which they developed vascularized skin graft utilizing human cells and 3D printing.
On the nature of this longstanding collaboration, Saltzman said, “We wanted to take [Pober’s] expertise on endothelial cells and my expertise on making materials and combine them to try and find new ways to make vascular networks in living animals. That collaboration has been going on for fifteen years, and we’ve had a lot of success. This is a start of something new, [and] I think it will take advantage of everything we’ve learned and push it in directions that will become clinically useful.”
The primary author of the paper, Tânia Baltazar, a Postdoctoral Associate in the Pober laboratory, studied biology as an undergraduate and went on to receive a master’s degree in biotechnology and a PhD in cell therapy and regenerative medicine in Lisbon, Portugal. “Tissue engineering is very application driven. You develop a product, and you can see the impact on the lives of patients,” Baltazar said, on why she chose to pursue the field. “I wanted to work on a project that would allow me to focus on regenerative medicine.”
This project was supported by the strong collaboration between the two research groups, as immunology and engineering came together to form a single product greater than the sum of its parts. Though Saltzman studied chemical engineering as an undergraduate student, he was not interested in ‘traditional’ chemical engineering careers, such as the petroleum industry. Instead, he chose to enroll in a program at MIT and Harvard Medical School that combined medical school training with engineering. “There weren’t a lot of formal programs in biomedical engineering at the time, but it gave me a way to use these tools to solve medical problems. It was a transformative experience,” Saltzman said.
Different Cells with Different Needs
This study, which tackles the long-standing problems of designing and implementing skin replacements for the treatment of cutaneous ulcers, originated as a collaboration between RPI and Yale, with a focus on in vivostudies within living organisms. The project began by considering why nonnative skin replacements, which do not come from the same individual, often fail to engraft within their hosts. This is tied to the lack of blood vessel connections—known as vascularization—between the skin and the implant. In other words, our body takes too long to perfuse the grafted skin with blood. Without of nutrients and oxygen, the implanted skin sloughs off. Adding a pre-vascularized bed into the graft accelerates the process of blood perfusion and enhances graft survival.
“This is a project where you have to combine four different cell types to construct a tissue, and each has very different needs,” Baltazar said. Tissue engineering skin substitutes do exist, but tend to function simply as “expensive bandages.” That is to say, while they protect wounds, they do not integrate and eventually lose their adhesive properties, because they cannot become vascularized like real skin. One example of this kind of skin graft is Apligraf TM. Another alternative to using tissue engineered constructs includes autologous grafting, a process by which a patch of skin is removed from elsewhere on the subject’s body and placed over the wound. Considering many patients suffering from cutaneous ulcers also suffer from diabetes, this method may result in a second injury the patient’s body is unable to heal.
“There were several hurdles in this project, some of which have been solved, others that have only been partially solved,” Saltzman said. While Baltazar was working on the project as a visiting scholar at RPI, one of the greatest challenges was the logistics of tissue storage and transport from RPI to Yale, where it would be implanted into the animal models. As they worked to develop the vascularized grafts, they often found that the constructs would contract following their implantation. “We had to consider the biophysics, making changes in how we produce the implants to minimize this effect,” Saltzman said. Luckily, surgical techniques improved as the project progressed. The research team moved from in vitro experimentation to implanting the grafts into mice, solving this issue with a combination of physiology and surgical techniques.
Bioprinting Skin Grafts
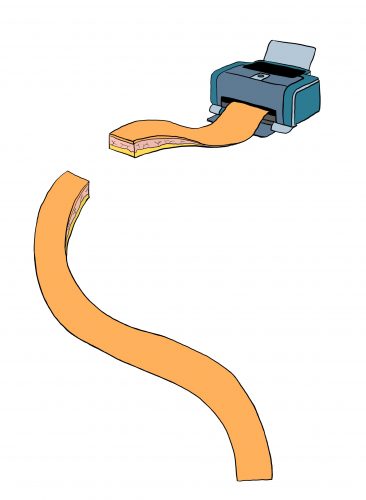
Utilizing 3D bioprinting technologies, the team successfully produced a skin graft that was both multilayered and vascularized, culminating in two bioinks. The first dermal layer combines human foreskin dermal fibroblasts, which are the cells responsible for synthesizing structural proteins such as collagen, as well as endothelial (skin) cells and placental pericytes, cells which wrap around vascularized endothelium, to form the dermal layer. The second epidermal layer contains human foreskin keratinocytes, cells which produce keratin, which typically composes hair, skin and nails. These keratinocytes form a barrier, protecting the vascularized tissue. Keratin itself is particularly resistant to scratching and tearing. After implanting these tissue constructs into immunodeficient mice, the micro vessels of the mouse inoculate with the implant and fully perfuse after about a month, ‘fusing’ the tissues from the graft and mouse.
This process is carried out through a relatively new technology known as bioprinting. Various forms of bioprinting, including inkjet and laser assisted printing, can be used to better replicate the minutiae of human skin, such as the capillaries. Inkjet printers are primarily used in large-scale products, while laser assisted printing is expensive and used for higher resolution projects. Bioprinting can be thought of as 3D printing using biomaterials, where structures are formed layer-by-layer through the deposition of bioinks—substances comprised of a variety of living cell types. These bioinks can mimic the extracellular matrix, have the unique capability to be printed as a filament, and can be produced at relatively mild conditions.
Off-the-Shelf Product
Finding solutions to the issue of skin ulcers is a crucial scientific endeavor, with more than seven million Americans suffering from the condition each year. Many of these cases result from venous stasis and diabetes, with patients often lacking the ability to efficiently heal their wounds. According to the researchers, while the generation and implementation of 3D bioprinted vascularized skin grafts has yet to be fully realized, it has the potential to become an ‘off-the-shelf’ clinical product with wide availability to the public.
To this end, the produced grafts must be compatible with the host immune systems. One method by which the research team has worked to eliminate immune responses to ‘non-self’ antigens from members of the same species is the implementation of CRIPSR/Cas9 gene editing. Within human endothelial cells, a gene codes for the expression of the human leukocyte antigen, or HLA, protein, which plays a critical role in the regulation of the human immune system. The research team has shown it is possible to delete this section of the genome within their skin grafts, potentially leading to implants which would altogether avoid host rejection. “One of the challenges is compatibility: is this skin graft going to be rejected when we implant it into a patient. We are trying to make a universal immuno-evasive vascularized skin graft, something you could have available as an off-the-shelf product,” Baltazar said.
Saltzman, whose background is in chemical engineering, is particularly excited by the potential integration of drug delivery systems into printed skin grafts and has already worked alongside Prober to publish works covering the delivery of drugs such as VEGF, or vascular endothelial growth factor. “This 3D printing technique allows us to apply drug delivery technologies, but in a much more sophisticated way. We can make gradients of delivery systems, deliver the drugs in different patterns, and I think that is going to be a very powerful part of the approach worth exploring,” Saltzman said.
About the Author: Matt Spero is a junior in Morse College pursuing the simultaneous B.S./M.S. degree in Biomedical Engineering. In addition to writing for the YSM, he is the president of both Yale Biomedical Engineering Society & Taps at Yale and is a researcher in the Human Nature Lab.
Acknowledgements: The author would like to thank Tânia Baltazar and W. Mark Saltzman for their time and enthusiasm.
Extra Reading:
Baltazar, T., Merola, J., Catarino, C., Xie, C., Kirkiles-Smith, N., Lee, V., … Karande, P. (2019). Three Dimensional Bioprinting of a Vascularized and Perfusable Skin Graft Using Human Keratinocytes, Fibroblasts, Pericytes, and Endothelial Cells. Tissue Engineering. Advanced online publication.