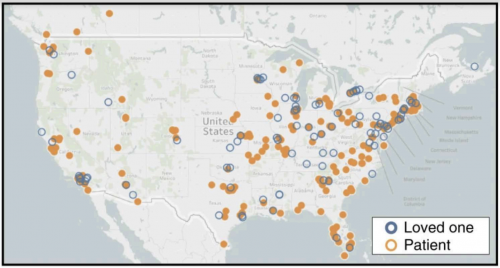
Map of Angiosarcoma Project Participants. The geographic spread demonstrates the advantages of this project in studying rare diseases. Photo courtesy of Painter et al., 2020.
The ultimate goal of clinical and translational research is to leverage scientific discovery and innovation to drive improved treatments and patient outcomes. In light of this goal, it seems reasonable that patients and the public should be involved in the research process. Yet, there is a disconnect between researchers and the public, even in translational settings.
There is increasing awareness of the necessity of patient and public involvement in both clinical and preclinical research. There are several disadvantages at play when these partnerships are absent. For one, scientists often lack personal experience with the diseases they study. As a result, they may not be attuned to the most pressing treatment needs in disease communities, potentially limiting their ability to translate knowledge production into knowledge use. In other words, lack of patient input on the research process can result in research waste––in which scientific communities produce research findings that have minimal real-world application. Moreover, given that a great deal of research is publicly funded, scientists have a duty to be accountable and transparent with the public. This is greatly facilitated by public involvement in research, which therefore has inherent democratizing value.
What is patient and public involvement?
The patient and public involvement (PPI) model is an approach that acknowledges the need to include patients and the public in research. PPI is flexible, and can consist of varying degrees of participation in the research process. Involvement often focuses on including patients in research design and in disseminating results. Less commonly, it encompasses participation in data analysis and methodological design. Significantly, PPI methods can be implemented in a broad range of research areas, from clinical studies and cancer research to groundbreaking research in the basic life sciences.
PPI offers several benefits over traditional research, which is executed solely by the investigating team of scientists. As implied by its name, PPI democratizes research by increasing the number of voices included in the research process. Researchers are optimistic that including public voices can produce studies that are more ethical and practical in nature. In health studies especially, patients can offer critical and overlooked perspectives in the research process. They can highlight aspects of the disease and treatment that are deprioritized in the academic community (such as drug-induced cytotoxicity), and also help researchers identify the most pressing pathobiological questions in the patient community.
Recently, PPI is gaining traction for its potential to address representational inequality in research. There is an extreme lack of representation in biomedical sciences and health professions. As a result, the unique health perspectives and grievances of minority populations are easily overlooked. Additionally, those who participate in clinical trials or experimental drug treatments are typically those with the best access to healthcare––most frequently, individuals who are affluent and white. These factors contribute to persistent disparities in health outcomes. PPI, by including a diverse patient population, can help foreground the health experiences of marginalized populations. Researchers who conduct PPI studies are aware of the need to increase diversity in research. While this awareness is encouraging, many of these researchers recognize that thus far, a majority of patient involvement in research is by wealthier white patients. Groups like the Community and Patient Partnered Research Network (CPPRN), which focuses on improving mental and behavioral health outcomes for Black and Hispanic populations, are working towards ensuring greater diversity in patient networks to overcome this challenge.
Finally, patient-centered research holds promise for improving the study of rare pathologies, including rare cancers. Rare diseases are difficult to study due to restricted availability of patient samples. Patient-centered approaches to rare diseases, by generating patient networks, can facilitate the collection of patient samples and data over a broad geographic range. This can compensate for the low frequency of disease incidence. The Count Me In initiative has spearheaded five projects involving patient-partnered cancer research. Recently, the initiative has launched The Angiosarcoma Project, which focuses on angiosarcoma—a rare, notoriously aggressive cancer that develops in the lining of blood and lymph vessels.
The Angiosarcoma Project: A model for PPI
The Angiosarcoma Project, with 338 patients, is the largest angiosarcoma project to date and has produced several novel and high-impact findings. The project was led by Corrie Painter of the Broad Institute. In the initial stages of the project, Painter ensured that patients were involved in the development of the online platform that would then be accessible to them and other patients. After receiving guidance from angiosarcoma patients, Painter and her team built out the project, received direct patient feedback, and synthesized that feedback in an iterative process. This serial generation-feedback-revision loop was done for everything seen on the Angiosarcoma Project Website (https://ascproject.org/).
Once the project was launched, high participation rates were almost immediate. After joining the project, participants could give consent to share online medical records, and send in saliva, blood, and tumor samples. Throughout the process, research updates were continuously disseminated to patients through the online platform, allowing patients to provide feedback.
Through the project, over forty-seven tumor samples were obtained, allowing for large-scale whole exome sequencing, a method that sequences protein-coding regions in the genome. Painter’s team could also access medical history data. Integrating these types of data enabled robust analysis of multiple subclasses of angiosarcoma. Sequencing data obtained for patient tumor-samples elucidated genes including TP53, KDR, PIK3CA, GRIN2A, and NOTCH2, that were consistently altered in angiosarcoma. Subsequent analysis of mutation frequency indicated that the PIK3CA gene is one of the most commonly mutated in breast angiosarcoma. This finding is clinically relevant, pointing to PIK3A inhibitors as a potential therapeutic route for primary breast angiosarcoma treatment. Finally, Painter looked at the tumor mutational burden, which is the number of somatic mutations in the DNA of cancer cells. She found that the number of mutations in head-neck-face-scalp (HNFS) angiosarcoma is significantly enriched, in a pattern consistent with UV-light induced DNA damage. This finding suggests that this angiosarcoma cohort might respond well to immune checkpoint inhibitors.
The novel findings produced by this project are already making an impact. “[Our project is] decoupled from the publication process entirely, so we’ve been releasing data for well over a year,” Painter said. By presenting at Clinical Oncology Alliance Meetings and to The American Society of Clinical Oncology (ASCO), Painter was able to share her results with clinical researchers. As a result, “there’s three different groups working on drafting clinical trials. One of them was able to get Angiosarcoma as a cohort in an existing checkpoint inhibitor study” she said. Painter also mentioned that two additional studies are being currently developed based on her data. Painter also anticipates the potential for pre-clinical researchers, who are not necessarily studying angiosarcoma, to see results from her project that involve pathways or genes of interest and being interested in partaking in angiosarcoma research.
The Angiosarcoma Project is a significant step forward for patient-partnered research. Painter demonstrated how a sincere and deep level of collaboration between patients and researchers can stimulate the most meaningful and translationally relevant results.
Challenges and future directions for PPI in research
Successful patient-partnered research, like the Angiosarcoma Project, is popularizing PPI. This is reflected in an increasing number of PPI studies, as well as the proliferation of grant applications that require researchers to describe how they plan to involve patients of the public in their studies. As this approach becomes more popular, it is important to consider current challenges and future directions of this type of research.
The single greatest challenge to expanding PPI in research is scientists’ lack of clarity on the most effective ways to facilitate engagement with patients. Painter, when discussing the Angiosarcoma Project noted that building the project, “was much easier than the metastatic breast cancer project because we were going off a vision.” For her, the Metastatic Breast Cancer Project, which was the first launched Count Me In project, provided a scaffold that was subsequently used to build out the Angiosarcoma Project in a way that was tailored to that specific patient community. Painter’s insight highlights how researchers can draw from previous studies in order to guide and facilitate their own PPI studies. Painter notes that it is imperative to adapt each project to the needs of the specific disease community, but that having a pre-existing vision is still highly useful.
As PPI expands, ensuring a continued commitment to patient diversity is critical. One way to facilitate this is by ensuring that patient-advocates from diverse backgrounds are included, since these advocates are the cornerstone of research outreach efforts.
Finally, while most research integrating a patient-centered approach involves clinical research or translational research that makes use of patient samples, there is a strong argument for patient-public involvement in pre-clinical and basic science research as well. Emma Dorris is a molecular biologist at The University College Dublin who also leads a PPI initiative for Arthritis Research. She argues that PPI elevates research by increasing the relevance and impact of projects. Dorris believes that patients can provide novel insights that direct scientists towards areas of a disease’s biology that haven’t been previously studied. While in a wet-lab setting patients cannot be involved in the data collection or analysis, there is a clear and meaningful space for their involvement in defining research questions and goals. In order to encourage researchers in preclinical labs to effectively integrate PPI, experts recommend training in patient-communication, as well as top-down incentives and infrastructure support from research institutions.
Patient-partnered research holds immense promise for biomedical science. It offers to improve the quality and relevance of research, improve relationships between researchers and the public, overcome boundaries to studying rare diseases, and help ameliorate racial and socioeconomic inequalities in research. As PPI studies continue to expand, critical examination of what types of engagement are most effective will be necessary.
Citations:
Burns, J. A., Korzec, K., & Dorris, E. R. (2019). From intent to implementation: Factors affecting public involvement in life science research. doi: 10.1101/748889
Jayadevappa, R. (2017). Patient-Centered Outcomes Research and Patient-Centered Care for Older Adults. Gerontology and Geriatric Medicine, 3, 233372141770075. doi: 10.1177/2333721417700759
Pii, K. H., Schou, L. H., Piil, K., & Jarden, M. (2018). Current trends in patient and public involvement in cancer research: A systematic review. Health Expectations, 22(1), 3–20. doi: 10.1111/hex.12841
Staniszewka, S. (2020). A patient–researcher partnership for rare cancer research. Nature Medicine, 26(2), 164–165. doi: 10.1038/s41591-020-0766-y