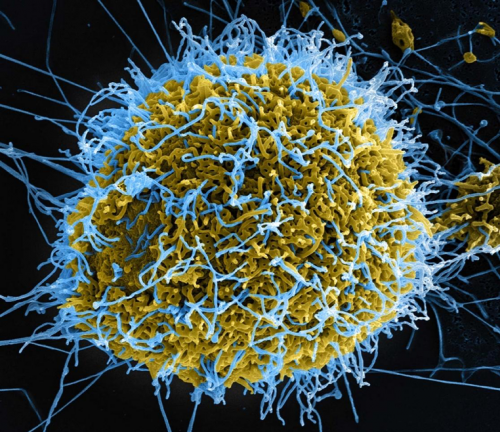
Image courtesy of Encyclopedia Britannica.
When we hear “Ebola,” we often think of its contagion and lethality, and of the outbreaks in recent years. Ironically, scientists are exploring the potential of the deadly Ebola virus (EBOV) as a treatment against a fatal form of cancer: brain tumors. Cancer cells lack the ability to generate an immune response against viruses, making viruses a good starting point for developing treatments. Of course, infecting someone with a lethal virus is risky; to circumvent this, scientists use chimeric viruses, which contain a mix of genes from multiple parent viruses. A team of researchers, including Yale professor Anthony Van den Pol, recently reported their efforts to test three variations of a chimeric virus, pairing an EBOV glycoprotein with the vesicular stomatitis virus (VSV). They chose the Ebola gene, given the virus’s propensity to infect—and for their purposes, target—nerve tissue. Specifically, they took interest in the mucin-like domain (MLD) of the Ebola virus, and how it modulates the viral ability to target brain tumors. Interestingly, it seemed as if the MLD protected normal cells from infection, while cancer cells still became infected. They were hopeful that VSV-EBOV could be a promising treatment, as the combination had been an effective and safe vaccine in humans during the African Ebola outbreak.
The team tested three viruses on severe combined immunodeficient (SCID) mice, which had human brain tumor cells injected into their brains: VSV-EBOV, which contains the mucin-like domain (MLD); VSV-EBOVΔMLD, which is a parallel construct but lacks the mucin-like domain; and VSV-EBOVΔMLD-GFP, which is almost identical to VSV-EBOVΔMLD with an added green-fluorescent protein (GFP) reporter gene to visualize a virus. All three showed some increase in the mice’s survival. The researchers found that the VSV-EBOV was most effective in treating the brain tumors while maintaining the health of the mouse. At 120 days after the tumor implant, only mice infected with the MLD-containing virus remained alive.
The researchers considered VSV-EBOV successful because it minimally infected healthy neural cells while still targeting tumor cells. Van den Pol’s team quantified the extent of the brain infection by counting the number of infected neurons and glial cells in coronal brain sections. The other two virus forms showed widespread infection throughout the brains of the animals. The VSV-EBOVΔMLD-GFP was the least effective. While it modestly extended the survival of the mice, all of the mice died. Some were incompletely infected by the virus, and many still had brain tumors. The VSV-EBOVΔMLD injected tumors had similar tissue structure, and a greater survival rate.
The lethality of the VSV-EBOVΔMLD-GFP virus may have been due to the VSV backbone itself; this differs from those of the non-GFP chimeric viruses in all four of their base proteins, which may alter the behavior of the virus. Van den Pol explained that the Ebola virus may release the MLD as a “false leader, causing the immune system to be lured away from the infected cells.” This slowed replication of the virus and lessened the amount of infectious viral offspring. With a slower replication rate, the innate immune system has more time to upregulate antiviral defenses. The low number of infected normal cells suggested that the innate immune system was sufficient to prevent the spread of the virus.
Researchers also compared the effects of intravenous versus intracranial injection. Both methods had degrees of success. Intracranial injection showed greater tumor infection and elimination, indicating this type of delivery may be more reliable for treating larger tumors. Intravenous injections, which are done through the tail-vein in mice, could on the whole be more effective for smaller or undetected types of metastatic cancer, such as melanomas.
Van den Pol and his team were able to monitor the impact of the MLD on the treatment and survival of SCID mice. The chimeric virus containing the mucin-like domain, VSV-EBOV, was the most successful treatment, confirming their initial expectations. This research is promising, as it could open the door for new forms of glioblastoma treatment. “VSV-EBOV has been successfully used in the human population in the past, showing that it’s relatively safe. If we’re ultimately trying to move toward clinical studies, that’s a hurdle already jumped over,” Van den Pol said. Future directions include looking at tumors in immunocompetent mice or exploring other VSV-based viruses.