Memory loss. Frustrated struggles to piece together past events. Forgetting the names of loved ones. These are likely some of the first symptoms that come to mind upon hearing the word “Alzheimer’s.” As a neurodegenerative disease, Alzheimer’s is characterized by a progressive loss of neuronal function that ultimately results in neuron death. This degeneration is responsible for the deterioration in cognitive and functional abilities associated with disease progression.
The devastating toll of Alzheimer’s—a currently incurable and extensively debilitating illness—touches thousands of American families every year, with over six million current cases in the U.S. alone. As the population ages, the number of Americans living with this condition is projected to reach 13.8 million by the year 2060. Yet, despite afflicting so many people, the complex puzzle of Alzheimer’s disease and the quest for how to treat it remains largely unfinished.
The progressive accumulation of a protein fragment known as amyloid-beta (Aβ) in brain regions important for cognition has long been believed to be the underlying cause of the neurodegeneration, neuronal death, and cognitive decline seen in Alzheimer’s. However, components of this hypothesis have been critically questioned, such as the scientific community’s understanding of the role of Aβ in Alzheimer’s and its relationship with other neuropathological hallmarks.
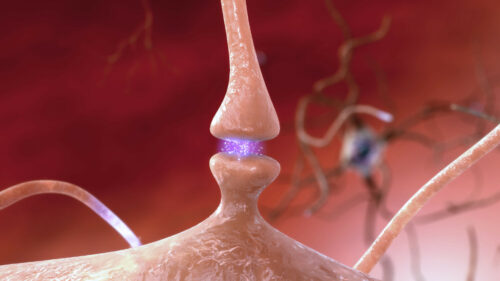
Beyond Aβ, synaptic loss, or the reduction of connections between neurons, has been described as the strongest neuropathological correlate with cognitive impairment in Alzheimer’s. Prior to this study, however, there had been no known publications investigating this relationship in living people, as previous work focused almost exclusively on postmortem analyses.
To fill in these gaps, a group of researchers at the Yale Alzheimer’s Disease Research Unit (ADRU) recently conducted an in vivo positron emission tomography (PET) imaging study, imaging the brains of living humans to investigate the relationship between Aβ deposition and synaptic density in the early symptomatic stages of Alzheimer’s. Because PET is an imaging technique that uses radioactive tracers, this allows scientists to detect and analyze Aβ deposition in people living with Alzheimer’s disease.
“The synaptic density PET tracer came out very recently, and now we can look in vivo at a live brain to study the relationship between synapse and Aβ,” said Christopher van Dyck, director of the ADRU and a co-author of the paper. There were two tracers used in this study: one that allows for the measurement of synaptic density and a second that allows for the quantification of Aβ in the brain.
Although the clinical presentation of Alzheimer’s spans a broad range of cognitive and functional deficits, the focus of this study was on early stages of the disease, which are known as the prodromal and mildly symptomatic stages. Importantly, while Alzheimer’s can only be definitively ascertained after death through an autopsy of the brain, it can still be clinically diagnosed using a thorough clinical history, neurological examinations, and magnetic resonance imaging (MRI), which can help rule out other contributing causes that could generate similar symptoms. “The autopsy report demonstrating those Aβ plaques, that was the gold standard diagnosis of Alzheimer’s for a long time, but you can still clinically diagnose Alzheimer’s disease without autopsies today,” van Dyck said.
Aβ Deposition and Synaptic Density
While the full physiologic role of Aβ is still unknown, it is understood that pathologic Aβ forms from the sequential division of a protein called amyloid precursor protein. These Aβ protein fragments then aggregate and ultimately form larger Aβ fibrils outside of cells. This insoluble fibrillar Aβ is what comprises amyloid plaques, the large deposits of Aβ outside of cells that are characteristic signs of Alzheimer’s.
Over time, the deposition of fibrillar Aβ in the brain is thought to approach a plateau. “I like to think of it as sort of an equilibrium; it reaches a point where you’re accumulating amyloid at the same rate as you’re clearing it, and fibrils are aggregating at the same rate they’re being cleared,” said Ryan O’Dell, first author of the paper and a fourth-year resident in the Yale Department of Psychiatry.
Although the presence of Aβ deposition is certainly a pathologic hallmark of Alzheimer’s, Aβ plaque buildup is generally not well correlated with measures of either disease severity or symptom duration. “Even in early studies when we only had autopsy reports to base off of, amyloid plaques tended to correlate relatively poorly with any index of disease severity,” van Dyck said. These observations are likely due to the deposition of Aβ reaching the aforementioned ceiling, at least in later stages of the disease.
With the advent of Aβ PET imaging and the ability to longitudinally track the in vivo accumulation of Aβ over time, the definition of this “plateau” has become more refined. Specifically, the continued accumulation of Aβ has been demonstrated through the early, prodromal stages of Alzheimer’s, with minimal accumulation by the time of conversion to dementia.
Therefore, the authors postulated that in the earlier stages of Alzheimer’s—when Aβ is still accumulating—there would be an observed association with measures of disease severity, including synaptic loss. In addition, they hypothesized these associations would be strongest in brain regions characterized by early synaptic loss, such as the hippocampus.
In this study, the primary analysis focused on the relationship between Aβ deposition and synaptic density in the hippocampus, a brain region that plays an important role in the consolidation of long-term memories and that is marked by early synaptic loss in Alzheimer’s. “Synaptic density is the best correlate of cognition, which makes it important to being able to look at a person with Alzheimer’s disease and evaluate how well their memory and cognitive function are working,” van Dyck said.
Participants were placed into three distinct groups after completing a series of clinical interviews, cognitive tests, and brain scans. The study enrolled 57 individuals—19 who were cognitively normal (CN), 14 with amnestic mild cognitive impairment (aMCI; an earlier prodromal stage) due to Alzheimer’s, and 24 with mild Alzheimer’s dementia (a more advanced, albeit still mild clinical stage). An important distinction between the CN group and the aMCI and dementia groups was that all CN participants were characterized by an absence of Aβ deposition, as assessed by the Aβ PET imaging, while all aMCI and dementia participants were classified as positive for brain amyloid. Additionally, and as expected, participants with aMCI exhibited less severe cognitive impairment than those with dementia.
Relationship Between Aβ Deposition and Synaptic Density
Consistent with the researchers’ primary hypothesis, there were statistically significant results demonstrating an inverse association between global Aβ deposition and hippocampal synaptic density within aMCI participants, but not within participants with dementia. These findings lend support to the model that Aβ continues to accumulate in the early stages of the disease before approaching a plateau, a point at which Aβ may uncouple as a primary contributor to the ongoing neurodegenerative processes, including synaptic loss.
However, the authors recognized that the study’s overall findings are limited by its small sample size and the lack of longitudinal data gathered over a longer time. Including this kind of data could allow for a more powerful analysis of the relationship between Aβ deposition and synaptic density across the Alzheimer’s disease clinical continuum.
Extending Our Understanding of Aβ and Synaptic Density
Although this study showed an inverse relationship between global Aβ deposition and hippocampal synaptic loss in the early, prodromal stages of the disease, this relationship was not generally observed across other brain regions. This opens the door to future molecular imaging studies of Alzheimer’s.
Thus, while past postmortem and in vivo imaging studies have shown that Aβ is not generally well correlated with disease severity, other pathologic proteins associated with Alzheimer’s, such as the hyperphosphorylated tau protein, may have a more specific regional relationship with synaptic density. Ongoing PET imaging studies at the ADRU are investigating this relationship between synaptic density and structures known as tau tangles, and this direction is promising.
Modifications to the current study could also allow for a more comprehensive understanding of the relationship between Aβ deposition and synaptic density across the clinical continuum of Alzheimer’s. “We are also interested in longitudinal work, which is one of the limitations of this study, because this would allow us to measure these markers of synaptic density, of amyloid, over time… allowing us to see not only how those individual proteins and measures change over time but also how their relationship changes over time,” O’Dell said.
Additionally, these investigations into the longitudinal relationship between synaptic density and other pathologic hallmarks of Alzheimer’s are currently being expanded into the preclinical, or symptomatically silent, stage of the disease. “The other big project that is really exciting is looking at a preclinical model of Alzheimer’s,” O’Dell said. “These would be participants who are younger than our typical cohort, maybe in their fifties or sixties, and have no subjective or objective cognitive impairment, but who are biomarker positive, confirmed by either PET imaging or fluid biomarker testing, for these pathologic amyloid and tau proteins.”
Alzheimer’s disease is devastating; it progressively destroys the control center of the human body to the point that it can no longer function normally. But there is much optimism in the advancing field of Alzheimer’s research. Research like this helps shed light on the complex relationship between Aβ and synaptic density in this disease, bringing us closer to fitting one more piece in the complex, unfinished puzzle of Alzheimer’s disease.
About the Author: Rayyan Darji is a first-year student in Grace Hopper interested in studying neuroscience on the pre-med track. In addition to writing for YSM, Rayyan is involved with Alzheimer’s Buddies, Yale Muslim Students Association, and Refugee and Immigrant Student Education.
Acknowledgements:
The author would like to thank Ryan O’Dell and Christopher van Dyck for taking the time to speak and discuss their research with him.
Supplemental Reading:
O’Dell, R.S., Mecca, A.P., Chen, MK., Naganawa, M., Toyonaga, T., Lu, Y., Godek, T.A., Harris, J.E., Bartlett, H.H., Banks, E.R., Banks, Kominek, V.L., Zhao, W., Nabulsi, N.B., Ropchan, J., Ye, Y., Vander Wyk, B.C., Huang, Y., Arnsten, A.F.T., Carson, R.E., & van Dyck, C.H. (2021). Association of Aβ deposition and regional synaptic density in early Alzheimer’s disease: a PET imaging study with [11C]UCB-J. Alzheimer’s Research & Therapy, 13(11). https://doi.org/10.1186/s13195-020-00742-y
Mecca, A.P., Chen, MK., O’Dell, R.S, Naganawa, M., Toyonaga, T., Godek, T.A., Harris, J.E., Bartlett, H.H., Zhao, W., Nabulsi, N.B., Vander Wyk, B.C., Varma, P., Arnsten, A.F.T., Huang, Y., Carson, R.E., & van Dyck, C.H. (2020) In vivo measurement of widespread synaptic loss in Alzheimer’s disease with SV2A PET. Alzheimer’s & Dementia, 16(7), 974–82. https://doi.org/10.1002/alz.12097