Image Courtesy of Flickr.
The possibility of rewriting genetic code has given hope to the 35,000 Americans suffering from cystic fibrosis (CF). In individuals with CF, a mutated gene causes a specific protein called the cystic fibrosis transmembrane conductance regulator (CFTR) to malfunction, wreaking havoc on the respiratory system.
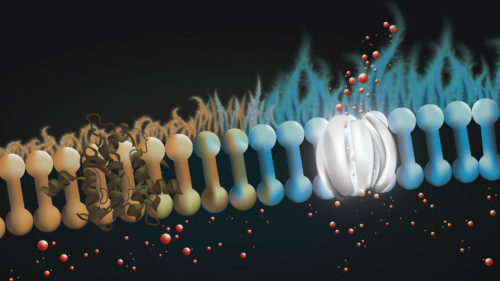
In each breath, dust, allergens, and pathogens enter our lungs and become trapped in a thin layer of mucus. This mucus must be constantly replenished to clean our airways and digest food, but without the properly functioning CFTR protein, mucus becomes viscous and thick, trapping contaminants in the lungs. The symptoms of CF manifest as coughing fits, frequent lung infections, and other discomforts. However, with the advent of gene editing, there is hope for a treatment for CF and other genetic diseases.
A recent study by Yale postdoctoral research fellow Alexandra Piotrowski-Daspit and Marie Egan, a professor at the Yale School of Medicine, investigated a novel gene editing approach to restore the function of the mutated CF gene in mice. They targeted a specific mutation, the F508del mutation, responsible for about ninety percent of CF cases. To edit the mutated gene, the researchers encapsulated peptide nucleic acids (PNAs) and an unmutated “donor” version of the CFTR gene into polymeric nanoparticles. PNAs are synthetic nucleic acids with a similar structure to DNA and the same complementary base pairs, which allow them to bind to target sites in genomic DNA. Once inside the cell, the PNA molecules form complexes around the mutated DNA, leveraging the cell’s natural repair mechanisms to insert the corrected sequence using the donor DNA as a template.
There are several key differences between PNA and CRISPR/Cas9 gene editing. CRISPR/Cas9 uses nucleases to “cut” genomic DNA, which reliably enables genetic modification, but may accidentally damage DNA in regions other than the target site. PNA-based editing reduces the possibility of off-target effects by harnessing the cell’s existing, non-mutagenic repair mechanisms to incorporate the correct DNA sequence. This makes them an attractive choice since they reduce the likelihood of accidentally harming other systems in complex living organisms.
The experiment demonstrated that gene editing has the potential to treat CF, which affects multiple organs throughout the body. “It’s kind of the holy grail of gene editing—to be able to effectively deliver gene editing agents systemically,” lead researcher Piotrowski-Daspit said. Even though the percent of cells edited in the treatment was less than the estimated five to fifteen percent needed to match healthy individuals, a partial restoration of function in the affected organs was observed without any off-target effects.
Looking beyond the specific F508del mutation that served as the focus of this study, new PNAs will need to be synthesized to target other mutations responsible for CF, for which no treatments are currently available. Piotrowski-Daspit’s personal goal is to improve delivery efficiency and restore function to a higher percentage of cells. These advances may eventually translate into treatments that can cure CF and other genetic diseases in humans.