Image Courtesy of Iva Knezevic.
The cancer world is buzzing about immunotherapies. They promise to target cancer cells while avoiding healthy cells, a difficulty for many cancer treatments since cancer cells often originate from mutated healthy cells. So with six hundred thousand people in the United States still dying from cancer every year, why are these therapies either not working in patients or not offered to them? Immunotherapies have recently shown promising results—but only in a handful of cancer types—and even then, they seem to elicit different responses between cancer patients depending on individual variability.
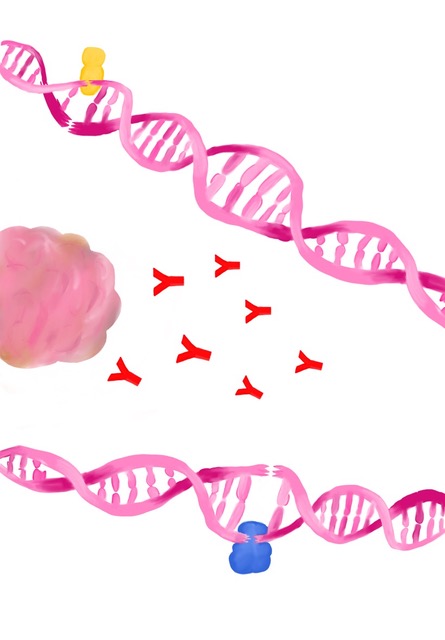
A new study completed in partnership between members of the Iwasaki Lab and the Santin Lab at the Yale School of Medicine analyzed data for endometrial cancer patients’ responses to immunotherapies. Immunotherapies are a type of cancer treatment that utilize the patient’s own immune system to fight cancer. Instead of using harsh substances such as chemotherapy or radiation to indiscriminately kill cancer cells, immunotherapy reactivates the body’s natural defense mechanisms to recognize and attack cancer cells.
“Immunotherapy is this really exciting area of cancer treatment where we use antibodies or other kinds of drugs to manipulate the immune system into better targeting cancer and recognizing it as something that needs to be eliminated,” said Ryan Chow, an MD-PhD student at the Yale School of Medicine and first author of the study.
A variety of different cancer immunotherapy approaches are actively being developed. Most clinical successes to date have been based on therapeutic antibodies that block specific proteins and receptors that allow cancer cells to evade the immune system. Other types of cancer immunotherapy include genetically modifying the patient’s existing immune cells to redirect them against tumors, as well as cancer vaccines that are analogous to those used for COVID-19 and other pathogens.
“The idea of immunotherapy is that our immune system is very good at dealing with foreign pathogens, things like viruses or bacteria, but in a way, we can also think of tumors and cancers as being foreign because they have acquired alterations and mutations that make them different on a genetic level,” Chow said.
While immunotherapies have improved survival rates for patients with certain cancer types, most patients do not respond to treatment. To date, the best response rates to immunotherapy have been seen in tumors with deficiencies in a DNA repair process called mismatch repair. Mismatch repair-deficient (MMRd) tumors characteristically accumulate very high levels of mutations, which in turn increases the probability that the immune system will successfully recognize the tumor as foreign. However, even among patients with highly-mutated tumors, less than half of patients will benefit from immunotherapy—a mystery that has long eluded scientists.
“Though taking the brakes off the immune system can be really effective, when you do that there can be intense side effects such as organ failure, autoimmune diseases—this is not a drug without its problems,” said Tai Michaels ʼ23, an undergraduate research assistant in the Iwasaki Lab and co-first author on the paper. Since the side effects of immunotherapy can be very severe, understanding why some patients are more or less likely to respond to treatment is key to maximizing the efficacy of immunotherapy while minimizing toxicity.
Two Subtypes of Tumors
Yale researchers studied the effects of immunotherapy on patients with endometrial cancer, a type of cancer that starts in the lining of the uterus. The team looked at twenty-four participants with different molecular subtypes of endometrial cancer—either mutational MMRd tumors (mut-MMRd) or epigenetic tumors (epi-MMRd). Six of the patients were classified as having mut-MMRd, which means that the driving mechanism of the cancer is mutations in the MMR genes, and eighteen were classified as having epi-MMRd, which means the driving mechanism of the cancer is epigenetic changes that silence mismatch repair mechanisms. Epigenetic changes are reversible changes that alter the way cells ‘read’ their DNA, but do not necessarily alter the DNA itself.
All patients were administered an immunotherapy called pembrolizumab—an antibody that blocks the inhibitory immune receptor PD-1—to evaluate its efficacy. Normally, the PD-1 receptor acts as a safeguard to prevent immune cells from aberrantly attacking the body’s own cells. As tumors can take advantage of this inhibitory mechanism to evade elimination by the immune system, blocking this receptor through anti-PD-1 immunotherapy can unleash an immune response against tumors.
The patients were treated with pembrolizumab every three weeks for up to two years. The researchers wanted to determine whether classifying patients by their mechanism of mismatch repair loss would allow them to better identify which patients are more likely to respond to anti-PD-1 immunotherapy. They observed that one hundred percent of the six mut-MMRd patients and forty-four percent of the eighteen epi-MMRd patients responded to the treatment, indicating that the mechanism of mismatch repair loss is indeed associated with the clinical effectiveness of anti-PD-1 immunotherapy.
“We used various sequencing techniques. Sequencing means trying to understand the DNA makeup of the cancer cells or looking at what kind of proteins or mRNA the immune cells are making, called [single-cell] RNA sequencing. By using a combination of the two, we were able to profile both the cancer and the immune cells in the same patients, so we can try to figure out after therapy, how the immune cells are reacting to certain types of cancer cells,” said Eric Song, an ophthalmology resident at the Yale School of Medicine and one of the lead senior authors on the paper.
The researchers also looked at peripheral blood mononuclear cells (PBMC) from patients before and after pembrolizumab treatment using single-cell RNA sequencing and matched T-cell receptor repertoire sequencing—a method of tracking T cells, immune cells that attempt to recognize and kill cancerous cells, and their specificities. PBMC samples are composed of a variety of immune cells that circulate in the blood, including T cells and natural killer cells, two major cell types which can be involved in mounting anti-tumor immune responses.
While the immune response in patients with mut-MMRd tumors was defined by T cells, that of patients with epi-MMRd tumors was instead characterized by natural killer cells. This led the researchers to conclude that the two molecular subtypes of endometrial cancer (mut-MMRd or epi-MMRd) are subject to different types of immune surveillance. This finding could, in turn, explain why patients with mut-MMRd tumors were more likely to respond to therapy, as the anti-PD-1 immunotherapy pembrolizumab is usually thought to act on T cells. At the same time, the researchers also discovered that natural killer cells from epi-MMRd patients demonstrated enhanced expression of many anti-tumor genes, suggesting that natural killer cells are the primary immune cells mediating anti-tumor responses in these patients.
What Next?
This study only analyzed twenty-four patients with one specific type of cancer, which raises the question of whether the conclusions would translate into a trend across other types of cancers and studies with larger patient cohorts. The researchers hope that the findings from this study could help inform further research on immunotherapies for various other cancers. Looking ahead, while this study was conducted on cancers with high mutational burdens, future studies could provide insight into cancers with variation in other factors—such as natural killer cell activation—and help improve the health outcomes of more cancer patients. “While mut-MMR patients had a uniformly high response rate, there was significant variation in response among epi-MMR patients which was not tied to mutational burden, suggesting that this was instead due to variation in other factors,” Michaels said.
While Chow and Michaels worked together on data analysis and curation, Song and colleagues led the study conceptualization and data collection. Along with the Santin lab’s team, who designed and enrolled patients in the clinical trial, their contributions all came together in the end. “It’s such a big team effort; it’s not something that one person can do alone,” Chow said. As teams of scientists across the world continue in this vein, immunotherapies could continue to improve the health outcomes of more and more cancer patients.