Image Courtesy of NIH Image Gallery.
It is well known that our risk for cancer increases as we age, but we still don’t understand why. How might the wrinkles marking the corners of our eyes relate to cancerous cells suddenly forming inside us? Previous research established a high correlation between cancer risk and the number of replications a cell undergoes throughout our life, leading to the hypothesis that random, unlucky mutations during cellular division are a notable driver of tumor formation. This aptly named “bad luck” hypothesis has been widely debated, with scientists questioning how the theory accounts for the impact of environmental factors. Now, researchers at Yale University are proposing an answer: an age-related chemical signature hiding in our genomes.
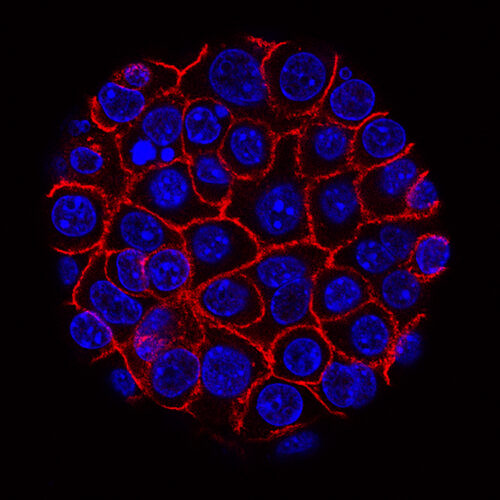
The study, conducted by recent PhD graduate Christopher Minteer and former Yale Assistant Professor Morgan Levine explores a set of epigenetic alterations called DNA methylation—that is, chemical attachments to the genome rather than changes within the DNA sequence itself—associated with aging and risk of diseases like cancer. Through the repeated replication of astrocytes, a type of cell found in the central nervous system ideal for this type of manipulation, Minteer’s team was able to mimic the rapid, unconstrained replication of tumorous cells. Having achieved tumor-like growth, the team then designed an algorithm to quantify the epigenetic signals in the cells. They eventually identified a progressive methylation signature that they called CellDRIFT, the strength of which increased with age across multiple tissues and differentiated tumors from normal tissue.
Through additional examination, Minteer’s team found that the CellDRIFT signature was elevated not only in cancerous cells, but also in healthy tissues that were predisposed to tumor formation. They examined healthy breast tissue from breast cancer patients prior to treatment and found that even the tumor-free tissues displayed an elevated CellDRIFT signature compared to non-cancerous controls, suggesting that CellDRIFT could predate the formation of tumors and serve as a warning sign. They also found that its presence was strongly correlated with poor patient survival, meaning that CellDRIFT, along with related measures, may help researchers and clinicians predict cancer aggression.
“We provided further context to the ‘bad luck’ hypothesis and created a tool to better study it,” Minteer said. While the “bad luck” hypothesis links the majority of cancer risk to random, sudden mutations in the genome, the CellDRIFT signature appears gradually. It slowly increases over time, meaning that CellDRIFT increments can vary depending on environmental factors, such as exposure to carcinogens. Thus, CellDRIFT can help provide a more thorough and unified understanding of the previously known underlying causes of tumor formation.
The researchers also explored whether they could reverse or otherwise reset the CellDRIFT signature. Namely, they manipulated stem cells to “reset” through a process known as Yamanaka factor reprogramming—a process in which special genes are introduced to cells to transform them back into an unspecialized state, thus allowing them to re-develop into new types of cells. Each instance of Yamanaka factor reprogramming consists of three phases: initiation, in which the cell begins to show genetic signs of resetting, maturation, in which the bulk of the reprogramming process occurs, and stabilization, in which the cells settle into their new form. Minteer’s team observed a dramatic decrease in CellDRIFT during the maturation phase, but the signature increased again once the cells entered the stabilization phase. In other words, they found promising evidence to suggest that although CellDRIFT cannot be stopped completely, it can be impeded, thus providing a new approach to preventive cancer treatments.
Minteer’s team also recognized that while CellDRIFT presence can be used to predict many aspects of cancer risk and aggression, calculating the signature is a difficult task in itself. Thus, they constructed a package to help clinicians and researchers quickly and efficiently quantify the signature, making their discovery more accessible to others unfamiliar with this field. “[The package] is uniquely suited to serve as a resource in the lab,” Minteer said. Although it still requires additional validation and experimentation, Minteer expressed excitement about the potential future uses of this package in both experimental and clinical settings.
While the use of epigenetic tools in clinics is still in its infancy, the findings of Minteer’s team are promising. CellDRIFT is unique in that it considers the myriad of factors that trigger the formation of an individual’s specific tumor, rather than reducing these factors to “just bad luck.” This provision of tailored cancer diagnoses makes CellDRIFT a compelling tool for clinicians to understand the full cancer narrative, and its contribution to the debate about cancer’s origin suggests a new, encouraging role for cancer prevention.