Art Courtesy of Madeleine Popofsky.
The great irony of recent advances in artificial intelligence (AI) is that even as programs have gained capabilities that ten years ago we could only dream of, most of the time, we have no idea how they do it. This lack of explainability has particularly frustrating consequences for the use of AI in drug discovery. Lacking the understanding of how AI generates predictions of successful drug candidates, scientists struggle to design drugs similar to those predicted. Felix Wong, a postdoctoral fellow at MIT, worked in collaboration with other researchers to solve this explainability problem in a recent Nature paper. The team applied newly explainable AI results to one of the most pressing medical crises of our age: antibiotic resistance.
Currently, bacteria are developing resistance to antibiotics at a rate that outpaces researchers’ ability to design new ones. “Antimicrobial resistance is a public health crisis that is projected to kill ten million people worldwide per year by 2050,” Wong said. An especially deadly enigma is methicillin-resistant Staphylococcus aureus (MRSA), which already kills over ten thousand per year in the United States. For researchers, MRSA has proved to be an elusive target. As a Gram-positive bacterium, S. aureus lacks an outer membrane that helps many bacteria defend themselves from antibiotics, but it has nevertheless independently evolved resistance to many antibiotics. Thus, to find an antibiotic for a bacterium as unique as MRSA, researchers would need to identify a whole new structural class of drugs—a tall order, given that gaps between such kinds of discoveries have previously exceeded thirty-five years.
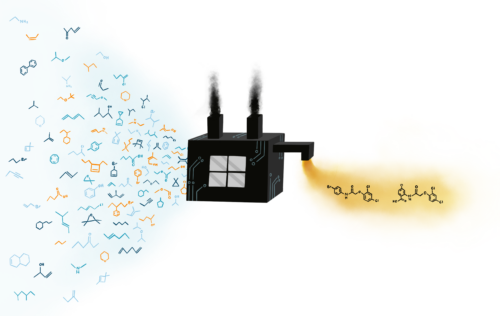
This is where AI steps in. Over the years, researchers have trained deep learning models, a type of AI, to identify certain desirable molecules that are linked to antimicrobial activity. Such models have limited success when researchers cannot identify the models’ reasoning—without it, researchers can’t point to specific chemical features that give the molecules their desired effects. These models are typically referred to as “black box” models.
Equipped with these standard “black box” models and determined to shed light on their inner workings, Wong and his colleagues took on the challenge of creating an antibiotic for MRSA. Their crucial insight was to focus on specific chemical substructures as units for the deep learning models. If a model focuses on specific substructures, Wong and his colleagues thought, then maybe they could get the model to explain which substructures in its chosen molecules account for its antimicrobial activity. During preliminary testing, this idea was confirmed. “We noticed that compounds with similar structures have consistently similar model prediction scores,” Wong said. The next step was to get the models to explain why these substructures matter.
To accomplish this, Wong and his colleagues started by manually screening nearly forty thousand compounds for their ability to inhibit MRSA growth and their toxicity to human cells. They then trained deep learning models on this data, testing the models with additional data afterward to ensure accuracy. Next, they fed over twelve million new compounds with unknown effects into these models. The models returned the compounds expected to have the best ability to inhibit MRSA growth with low toxicity to humans. Finally, the researchers applied a technique known as a Monte Carlo tree search, which performed the all-important task of identifying substructures responsible for the outputs of the models.
“We set out to see if we could ‘open the box,’” Wong said. In the end, the model used an algorithm similar to the one used in the game-playing AI called AlphaGo. While playing AlphaGo and identifying a new antibiotic class may seem like two very different processes, they have a key similarity: a need to search through an extremely large space of possibilities efficiently.
Armed with potential structural classes, Wong and his colleagues sorted through the data. They found explanations from the algorithm that matched the logic behind already identified antibiotic classes. However, the model also identified five different justifications for substructures that could potentially identify new classes. After narrowing down activity, they found that over forty percent of molecules within these newly identified classes showed activity that inhibited MRSA growth. All of these molecules were new to antibiotic researchers.
Further testing in the lab isolated the two best candidates, forming an entirely new class of antibiotics likely able to combat MRSA effectively in a clinical setting. These two compounds share a common substructure which was identified by the model as the source of their antimicrobial ability. Testing of their abilities in living organisms showed that they worked specifically against Gram-positive bacteria such as MRSA while avoiding injury of healthy cells. They kill bacteria by dissipating the pH gradient within them, causing them to burst open. The compounds succeeded in the tough task of killing MRSA in afflicted mice, showing promising clinical potential.
In identifying this new class, Wong and his colleagues opened the proverbial “black box,” finding a way to make deep learning algorithms explain their results using chemical substructures. While successful in explaining the properties that give a potential drug antimicrobial abilities, the model falls short in other areas. There are other important properties necessary for a potential antibiotic, including avoiding side effects such as hemolysis, the destruction of red blood cells, or genotoxicity, the damaging of DNA. Wong and his colleagues were forced to consider these possible side effects only after they had identified their new structural class. “Better predicting of all of these properties remains a critical challenge,” Wong said.
This process took two years, but since a large part of that time was spent developing the methodology, future research could take place considerably faster. Therefore, this new technique is a crucial new way to fight antibiotic resistance. “This discovery directly contributes to our arsenal of antibiotic candidates,” Wong said. “Our work also promises to accelerate antibiotic drug discovery by making deep learning models more explainable and providing publicly available large datasets and models that accurately predict selective antibiotic activity.”
Wong and his colleagues are currently working on using the substructure-based explanations given by AI to design new antibiotics from scratch. But impacts extend beyond just antibiotics. “We have also been continuing to develop and apply approaches like the one published here to discover other types of drugs—for instance, those that modulate aging and age-related pathways,” Wong said.
With the black box open, the future of antibiotic resistance is looking less bleak. “This is a very different approach from the one-target, one-disease approach prevalent in drug discovery, which typically aims to just optimize the fit of the small molecule against the target,” Wong said. “We can now […] provide a justification for why some molecules work better than others in a way that directly aims to produce the next generation of antibiotic candidates.”
In the end, when describing the process of reaching this crucial finding, Wong had only one word to use: “Exhilarating.”