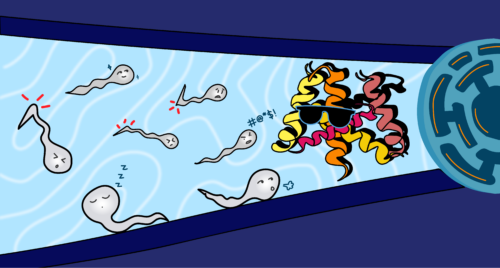
Art Courtesy of Luna Aguilar.
When sperm lose their ability to swim, the chances of conception take a dip as well. Around eighty percent of male patients with infertility have defects in their sperm motility, which refers to the sperm’s ability to move effectively and ultimately reach and fertilize an egg. Yet pinpointing the exact causes of these defects is surprisingly difficult.
In a recent study, researchers from the Yale School of Medicine and Quaid-i-Azam University in Pakistan collaborated to tackle this problem. “The majority of the mutations of these kinds of fertility genes are really hard to identify because, by nature, infertility genes or mutations affecting fertility don’t pass on to the next generation,” said Jean-Ju Chung, a senior author on the study.
Pakistani colleagues on Chung’s team collected blood and semen samples from the members of a family with hereditary male infertility caused by low sperm motility. Because the samples had similar genetics, it was easier to isolate which mutation was specifically tied to infertility. Using a type of DNA sequencing called whole exome sequencing, the scientists were able to identify a gene mutation that caused a defect in a protein component of sperm called leucine-rich repeat-containing 23 (LRRC23). LRRC23 was truncated, meaning the protein was cut short.
This left scientists with a question: how exactly might this defective protein cause infertility?
Demystifying the role of LRRC23
Using CRISPR/Cas9, a gene-editing technology that allows researchers to target specific DNA sequences, the team was able to reproduce the human mutation in mice. Then, they studied sperm cells from the animals via a computer-assisted sperm analyzer to measure sperm motility. Live sperm cells were recorded using a video camera and their movement was tracked using special software which calculated the velocity and path of each cell. The data showed exactly what the scientists expected: the sperm could not swim properly, and the mice were infertile.
“Biology is intricate and everything should be coordinated,” Chung said. Therefore, a structural defect in a single protein can affect the entire movement of the sperm.
Sperm swim using flagella—small, hair-like structures that beat back and forth to generate cell movement. Flagella are composed of nine sets of microtubules: hollow, tubular structures that run along the flagellum. These microtubules are connected in the core of flagella by T-shaped multiprotein complexes called radial spokes. Made up of “head” and “stalk” components, radial spokes are essential for controlling how the cilia and flagella beat—and by extension, controlling how sperm move.
The researchers demonstrated that the protein LRRC23 is a crucial head component of a specific radial spoke, radial spoke 3 (RS3). Chung’s team collaborated with the Zhang lab in Yale’s Department of Molecular Biophysics and Biochemistry to use a technique called cryo-electron tomography, a powerful imaging tool that bombards frozen samples with electrons to create high-resolution, three-dimensional representations of molecular structures. The advantage of cryo-electron tomography is that live samples can be observed on a highly magnified scale. “This technique is now the leading technique in structural biology,” Chung said.
Chung’s team was able to visualize the structure of sperm with and without the genetic mutation. In samples where LRRC23 was defective, the entire head region of RS3 was missing. This affected how the microtubules in sperm cilia and flagella interacted, leading to decreased sperm motility.
Flipping the script on LRRC23
Before this study, scientists thought that LRRC23 was a stalk protein rather than a head protein. Indeed, it was believed that LRRC23 was a homolog of the RS2 stalk protein RSP15—in other words, researchers thought LRRC23 and RSP15 shared a common ancestor and therefore might have similar functions. The problem, Chung’s team realized, was that RSP15 is a protein found in a type of algae called Chlamydomonas—and RS3 in Chlamydomonas doesn’t have a head component.
To put this long-held notion to the test, the scientists used biochemical analyses to track the evolution of LRRC23 and observe its interactions with other proteins. If LRRC23 were indeed a stalk protein, it would have been expected to interact with other known stalk proteins. Instead, it only interacted with head proteins.
“We actually found out that LRRC34, not LRRC23, looked like a mammalian RSP15 homolog, which conflicts with the major paradigm in the field,” Chung said. She and her team concluded that LRRC23 must be a head protein—specifically, a head component of RS3. This critical discovery gives researchers new insights into the structure and function of LRRC23.
The journey to this finding was not without obstacles. Halfway through the study, another research team published an article making similar connections between the gene Chung’s team was studying and male infertility. “It was disappointing in the moment,” Chung said. But Jae Yeon Hwang, the first author of the study, didn’t give up. He encouraged the team to continue studying LRRC23, and they ultimately discovered the protein’s role as a head rather than stalk protein. “We were able to make a different conclusion which turned out to be validated at multiple levels, including evolution, genetics, biochemistry, and structure,” Chung said. “It was a comprehensive and satisfying story as a scientist and highlights the power of interdisciplinary collaboration.”
But the story doesn’t end here. The team plans on pushing their work up to the atomic resolution. “Our next step is doing a proteomic study to really figure out the molecular composition and architecture of the radial spoke protein,” Chung said. This entails a comprehensive examination of all the proteins present in a biological sample, which will give researchers even more information about how exactly LRRC23 dysfunction causes male infertility.
Clinical implications
For Chung, the most satisfying part of her research is its potential translation into clinical practice. “This study in particular is linked to real, human patients,” Chung said. Identifying genes that reduce sperm motility will allow couples to be more informed about their fertility journeys. With a comprehensive, compiled list of genes causing fertility defects, clinics can conduct genetic screening to inform clients of their chances of conception. Further, they can tell couples if their future children might have a risk of being infertile when they grow up.
“By human nature, [couples] not only want to get treated, they also want to understand why they can’t conceive,” Chung said. Once couples have a better scientific understanding of why they might be infertile, it becomes easier to suggest treatment or new options for conception.
There is still hope for patients with defective LRRC23 proteins. A technique called intracytoplasmic sperm injection can be used on men who have low sperm motility. Intracytoplasmic sperm injection is a type of in vitro fertilization in which a healthcare provider chooses a healthy-looking sperm and uses a needle to inject this sperm directly into an egg. Then, the resulting embryo is transferred to the uterus of the female partner.
“The success rate may be low, but they can still conceive,” Chung said. “The process can be mentally, physically, and emotionally painful for women.” Chung hopes that her team’s work will lead to a better understanding of the regulatory mechanisms behind low sperm motility—and to better chances for conception.