Differences in CAR T-cell populations shed light on treatment efficacy
In a recent study published in Blood, scientists have begun to explain why CAR T-cell therapy is more effective for some patients than others. This research—a collaboration between Kite Pharma, a Gilead Company, and IsoPlexis Corp.—showed a correlation between CAR T-cell characteristics before treatment and the response of patients with non-Hodgkin’s lymphoma.
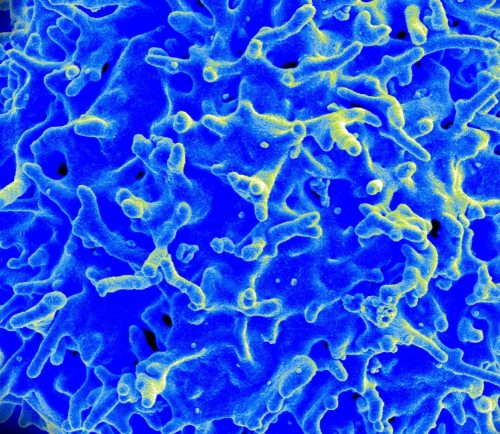
CAR T-cell therapy—approved last year by the FDA for patients—is used for the treatment of certain types of blood cancers. This therapy uses the patient’s own T-cells, immune cells that kill damaged or infected cells, to kill the cancer cells. A patient’s T-cells are removed and genetically engineered to target cancer cells using a chimeric antigen receptor (CAR). The newly engineered cells, now CAR T-cells, are then infused into the patient.
In the study, scientists analyzed patients’ CAR T-cells prior to infusion and compared the characteristics of the cells to the patients’ response to treatment. Using cutting-edge single-cell technology, the scientists found that CAR T-cells could be divided into five functional categories based on production of signaling molecules, with some cells fitting into more than one category (polyfunctional cells). The scientists then calculated a polyfunctional strength index (PSI), which represents the proportion of polyfunctional cells and the potency of these cells.
Both the PSI alone and the PSI combined with the ability of cells to grow correlated with the objective response of the patients to CAR T-cell treatment, indicating that a population of healthy, polyfunctional CAR T-cells improves the likelihood of a successful treatment. The scientists also determined that PSI combined with the ability of the cells to grow correlated with cytokine release syndrome, a condition of immune cell over activation that results in severe systemic inflammation. PSI of a specific CAR T-cell subset, inflammatory T17 cells, correlated with neural toxicity, where the nervous system is adversely affected. These findings show that a population of healthy, polyfunctional CAR T-cells increase the likelihood of a successful treatment but can also increase the likelihood of complications.
This study is just the beginning of understanding why patients respond differently to CAR T-cell therapy, and many questions remain. It is unclear how polyfunctionality is determined and if functionality can be changed. Because PSI and the ability of the cells to grow correlates with both objective response and complications, further study will be required to identify if patient response can be improved without substantially increasing the risk for complications.
According to John Rossi of Kite Pharma, the next step will be to do a larger trial and test their techniques in other types of blood cancers. “ALL [acute lymphoblastic leukemia] and lymphoma are different. You don’t know if the findings will be the same,” Rossi said.
Defining how CAR T-cell characteristics correlate with patient response has the potential to dramatically improve CAR T-cell therapy. “Learning mechanistically which T-cell subsets contribute to the efficacy of treatment and complications is the first step toward improving the therapy,” Rossi said. Using the information from these trials, it might be possible to alter the CAR T-cell production process or add therapeutic interventions that improve response or decrease the potential for complications.